CASE REPORT
https://doi.org/10.47811/bhj.167
Cardiotoxic effects of poisoning from aconite root in
a middle-aged man in Bhutan: a case report
Kuenga Sonam1,
Thinley Dorji2, Vivek Rai3, Kunzang Chophel5, Ugyen Chophel4, Choeda
Gyeltshen3, Nar Bahadur Rai3
1Kidu Medical Service
Centre, Thimphu, Bhutan
2Department of Internal
Medicine, Central Regional Referral Hospital, Gelephu, Bhutan
3Department of Emergency
Medicine, Central Regional Referral Hospital, Gelephu, Bhutan
4Wangdue Phodrang Hospital,
Wangdue Phodrang, Bhutan
5Department of Traditional
Medicine, Central Regional Referral Hospital, Gelephu, Bhutan
Corresponding author:
Kuenga Sonam
kuennam95@gmail.com
ABSTRACT
Introduction: Poisoning is a major
global health concern and a preventable cause of death. Aconite, an alkaloid
found in the aconitum genus frequently leads to poisoning in Asian countries
including Bhutan owing to its use in traditional medicine and religious items. Case
presentation: A 47-year-old male consumed a tincture of aconite plant root
and experienced vomiting, blurred vision, paraesthesia, and light headedness.
On presentation to the emergency department, his vitals were normal but on
subsequent close monitoring, he had premature ventricular contractions and
sinus bradycardia leading to hypotension and shock. He was admitted to the
intensive care unit for continuous cardiac monitoring and supportive treatment
including atropine and noradrenaline. He reported subjective improvement, his
vital signs improved and ECG returned to normal, enabling discharge after 5
days of admission. Conclusion: There is no specific antidote to aconite
toxicity so the treatment is mainly supportive. It is imperative to implement
proactive measures such as public awareness programs and dedicated research
efforts to mitigate the risk of inadvertent toxicity resulting from aconite
use.
Keywords: Aconite; arrhythmia; cardiotoxicity;
neurotoxicity; plant poisoning
Poisoning
represents a common preventable cause of morbidity and mortality worldwide.
According to the World Health Organization, unintentional poisonings were
responsible for about 84,000 deaths in 20191. Aconite, also called Aconitum, is
an alkaloid found within the Actinium genus. The plant is also referred to as
monkshood, wolfsbane, or the queen of all poisons. Aconite poisoning is
predominantly reported in Asian countries like China, India, and Japan due to
its historical use in traditional medicine. Between 2001 and 2010,
approximately 5000 instances of aconite poisoning were documented across these
nations2. Bhutan also witnesses aconite poisoning given its centuries-old
utilizations as both poison and an ingredient in traditional medicines. The clinical
manifestations of aconite toxicity can vary widely and may lead to severe
outcomes including fatality.
We report a case of aconite poisoning in a
lay monk who presented in June 2023 to our hospital in Gelephu, Bhutan.
CASE PRESENTATION
A 47-year-old male, who was previously
well with no known comorbidities presented to the emergency department with
vomiting, blurring of vision, paraesthesia, and light-headedness. He had
ingested a tincture of aconite plant root (Figure 1) approximately 4 hours
prior to hospital presentation. He was a lay monk and ingested the plant root
to check if it was viable before offering it on the altar.

Figure
1. A small piece of the root of Aconite plant that had been collected from the
forest for the purpose of adding it as an ingredient to religious ceremonial
items (Photo shared by the victim)
On admission, his Glasgow Coma Scale
score was E4V5M6 (15/15). He was diaphoretic, agitated, and anxious. His pulse
rate was 70 beats per minute, blood pressure was 120/80 mmHg, and peripheral
oxygen saturation was 100% on room air. Cardiovascular examination revealed
normal heart sounds. The respiratory system examination showed bilateral
vesicular breath sounds. The abdomen was soft and non-tender, with no
organomegaly and normal bowel sounds. The nervous system examination revealed
no focal neurological deficits.
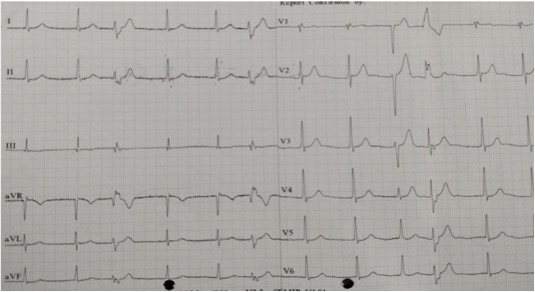
On presentation, a 12-lead electrocardiogram (ECG) showed
junctional rhythm with premature ventricular complexes. (Figure 2).
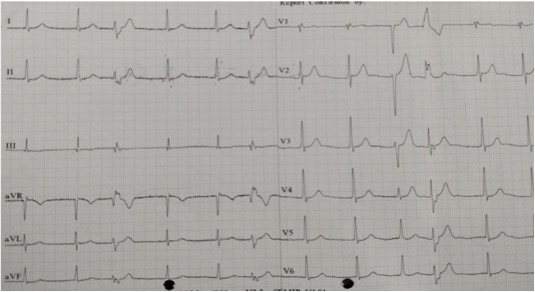
Figure 2. ECG at
presentation: junctional rhythm with bidirectional premature ventricular
complexes.
A comprehensive blood workup (Table 1) revealed values within
the normal range.
Table 1. Summary of laboratory investigation findings
of a 47-year-old make treated for cardiotoxicity following consumption of root
of aconite plant.
|
Laboratory investigations
|
Test results
|
Reference range
|
|
Complete blood count
|
|
White cell count (*10^3/µL)
|
8.30
|
4.0-10.0
|
|
Lymphocyte (%)
|
26
|
20-40
|
|
Neutrophil (%)
|
69
|
40-60
|
|
Haemoglobin (g/dl)
|
14.7
|
14.0-18.4
|
|
Platelet (10^3/µL)
|
238
|
150-450
|
|
Liver function test
|
|
AST (IU/L)
|
27
|
0-35
|
|
ALT (IU/L)
|
40
|
0-45
|
|
Total Bilirubin (mg/dL)
|
1.4
|
0.2-1.0
|
|
Direct Bilirubin (mg/dL)
|
0.3
|
0.0-0.2
|
|
Renal function test
|
|
Urea (mg/dL)
|
28
|
15-45
|
|
Creatinine (mg/dL)
|
1.0
|
0.6-1.3
|
|
Electrolytes
|
|
Sodium (mEq/L)
|
148
|
135-145
|
|
Potassium (mEq/L)
|
3.0
|
3.6-5.0
|
|
Chloride (mEq/L)
|
115
|
96-110
|
|
Coagulation studies
|
|
PT (s)
|
15.7
|
13.6-17.5
|
|
INR
|
1.2
|
0.8-1.2
|
|
Venous blood gas
|
|
pH
|
7.45
|
7.35-7.45
|
|
pCO2 (mmHg)
|
36.8
|
35-45
|
|
pO2 (mmHg)
|
37.9
|
95-100
|
|
HCO3 (mEq/L)
|
24.7
|
22-26
|
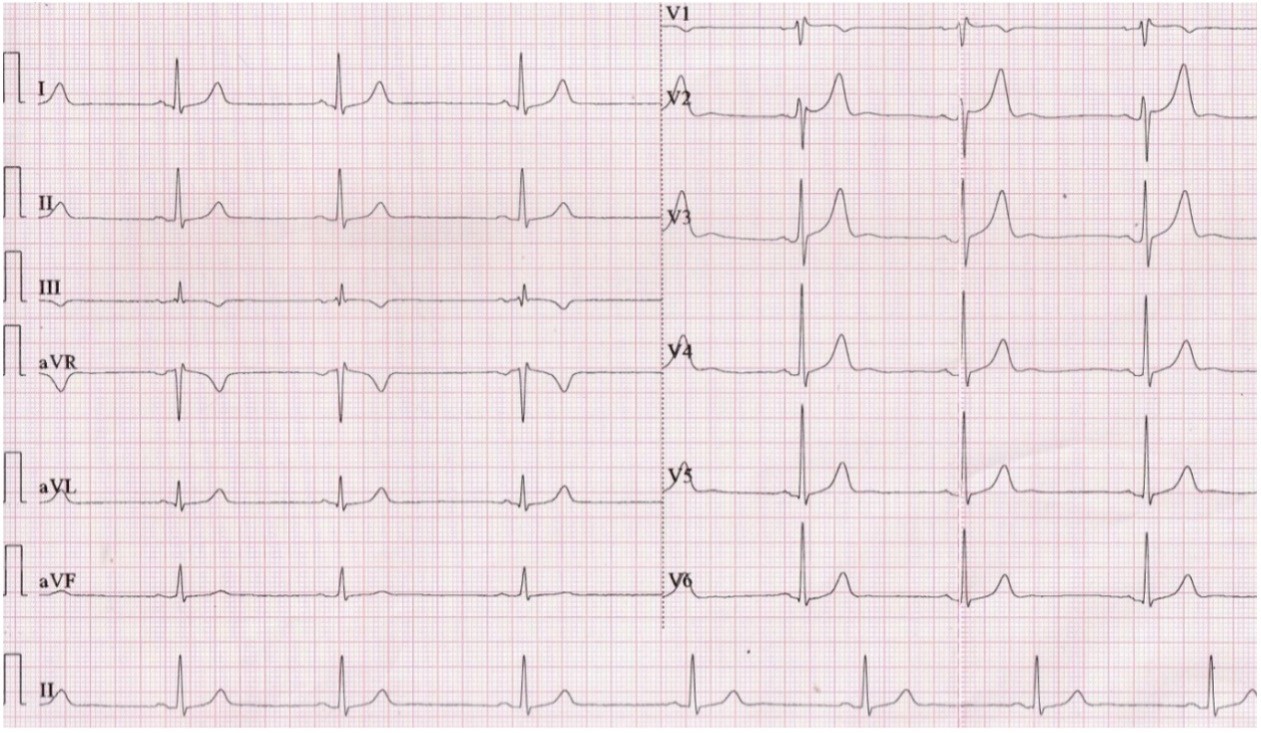
Considering the history of aconite ingestion followed by
symptoms suggestive of cardiotoxic effects, the patient was admitted to the ICU
for continuous ECG monitoring. During the course of monitoring at the ICU, he
developed a syncopal episode during which his heart rate dropped to 40 beats
per minute with a blood pressure of 80/60 mmHg. ECG at that point revealed
sinus bradycardia (Figure 3). In response, two doses of intravenous atropine
0.6mg each were given, five minutes apart. Due to persistent hypotension
despite a 1000ml bolus of crystalloids, noradrenaline infusion (0.1mcg/kg/min)
was started and continued for about 12 hours to maintain mean arterial pressure
> 65 mmHg. Although the choice of drug for chemical pacing is either
adrenaline or dopamine, noradrenaline was the only agent available at the time.
He had about 20 bouts of vomiting resulting in hypochloraemia and hypokalaemia.
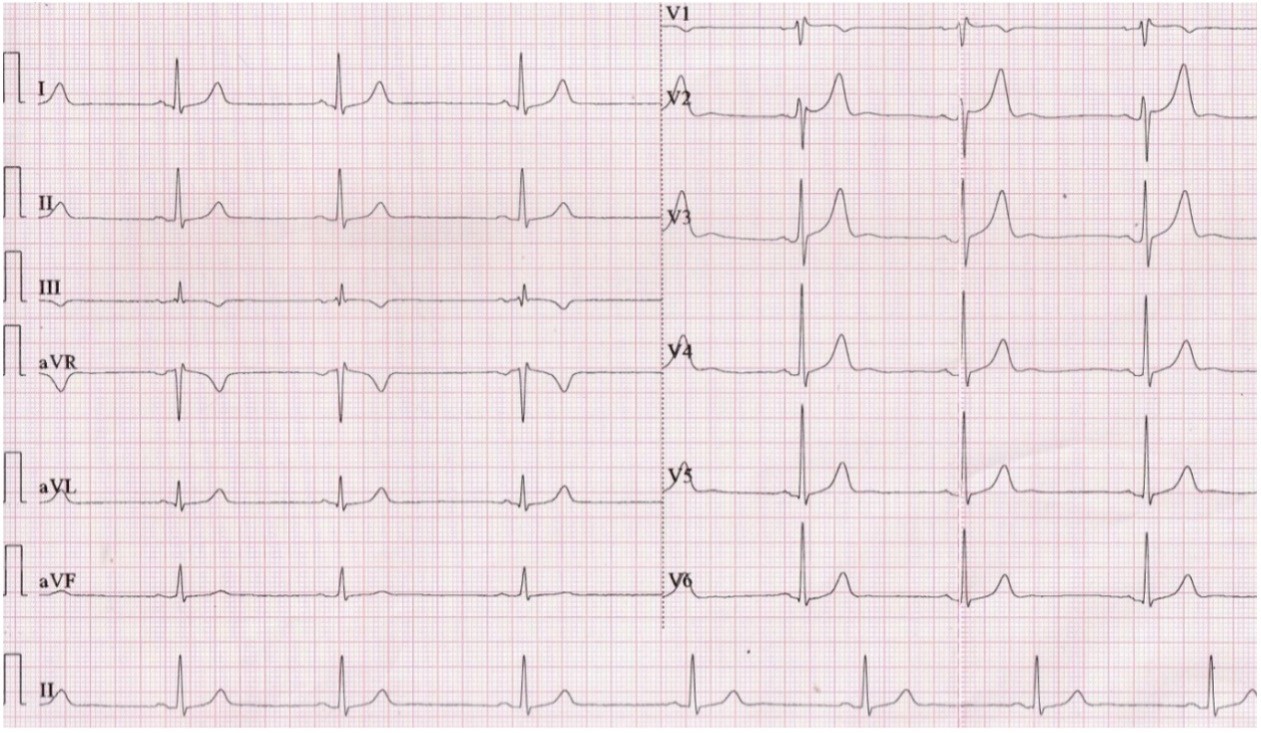
Figure 3. ECG showing sinus bradycardia
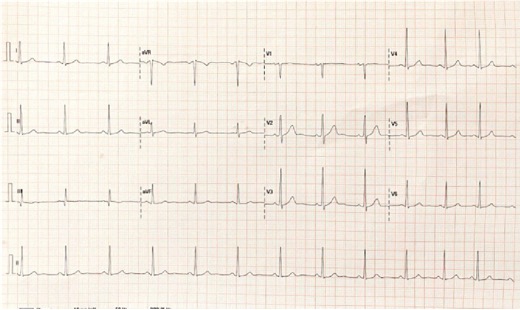
Forty-eight hours into ICU admission, vomiting had resolved
and vital signs had returned to normal. Noradrenaline infusion was tapered off.
Continuous monitoring of ECG revealed the presence of sinus arrhythmia. He was
transferred to the Medicine Ward for observation and was discharged home 3 days
later. At his one-week follow-up at the outpatient clinic, he was symptom
free, his ECG had reverted to normal sinus rhythm (Figure 4) and 2D
echocardiography showed normal cardiac function.
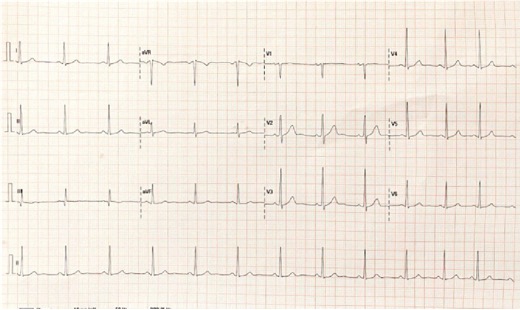
Figure 4. ECG on one-week
follow-up: Normal sinus rhythm
DISCUSSION
The scientific name of aconite or monkshood is Aconitum. This
group comprises more than 250 species of flowering plants that belong to the
Renunculaceae family. Aconite is utilized in medicinal practices in Asian
countries like China, Japan, India, and Bhutan. In Bhutan, it is referred to
as Tsenduk, Menchen, or Bonga. Various parts of the aconite plant are used for
different purposes, primarily in traditional medicine practices. It is used as
a constituent in over 25 medicinal preparations of Bhutanese traditional
medicines that are used for their analgesics and antiinflammatory properties3.
It is also used for other purposes such as poison in hunting wild animals and
offerings during rituals. The toxicity of the extracts corresponds to its
alkaloid content that is present in its roots, flowers, leaves, and stems. The
most common route of exposure is oral ingestion.
Aconite poisoning is primarily diagnosed on clinical grounds.
It is suspected in patients with a history of consuming parts of the plant and
exhibiting symptoms of toxicity. Aconite is a rapidly acting toxin, and
individuals who have been poisoned by it typically exhibit a constellation of
symptoms encompassing neurological, cardiovascular, and gastrointestinal
manifestations4. Neurological symptoms such as paraesthesia, numbness, and
burning sensations in the lips, tongue, and mouth are felt almost immediately
after ingestion. These are followed by cardiovascular symptoms like
palpitations, syncope, and dizziness. Gastrointestinal symptoms, including
nausea, vomiting, abdominal pain, and diarrhea, may also occur. Additionally,
individuals may experience visual blurring, yellow-red color vision distortion,
and coordination difficulties. Severe cases may lead to refractory arrhythmias
and refractory hypotension, potentially resulting in sudden death. Literature
reports an in-hospital mortality rate of 5.5% with acute aonite poisoning5. Two
cases of unintentional aconite poisoning with cardiotoxicity were reported in
Bhutan following the consumption of aconite-containing traditional medicine3.
C19-diterpenoid alkaloids, notably aconitine, mesaconitine,
and hypaconitine, constitute the primary toxic components within aconite roots4,6.
These potent alkaloids exert their toxicity by targeting voltage-sensitive
sodium channels present in excitable tissues such as the myocardium, nerves,
and muscles. This action leads to the prolonged activation of these channels,
preventing their normal inactivation process. Consequently, there is a
continuous influx of sodium, resulting in sustained depolarization that renders
the tissue refractory to further excitation. Furthermore, aconite inhibits
Sodium Potassium ATPase, prolonging the influx of sodium and sustaining
depolarization. Activation of the Sodium Calcium Exchanger by aconite leads to
an increase in cytoplasmic calcium levels, disrupting excitation-contraction
coupling and precipitating arrhythmias7.
Aconite’s interaction with the human ether-a-go-go related
gene channel (hERG) influences action potential duration; its blockade of hERG
channels prolongs action potential duration, contributing to arrhythmias such
as ventricular ectopics, ventricular tachycardia, torsades de pointes,
ventricular fibrillation, and even death7. Aconite’s propensity to
induce irregular heart rhythms has also been linked to its anticholinergic
effects, mediated through the vagus nerve.
Furthermore, aconite also acts on the ventromedial nucleus in
the hypothalamus which regulates the autonomic nervous system causing
bradycardia and hypotension6.
Toxicological analysis of aconite can be performed to detect
the presence of aconitine or its metabolites using techniques such as liquid
chromatography mass-spectrometry and immunoassays8. However, it is
not available in Bhutan and diagnosis is mainly based on clinical grounds.
There is no specific antidote to aconite poisoning and
management is mostly supportive. Hypotension can be managed with the
administration of intravenous fluids and vasopressors. Various arrhythmias
necessitate tailored management approaches. Bradycardia is typically addressed
with atropine. For ventricular arrhythmias linked to aconite poisoning,
amiodarone and
flecainide as preferred first-line antiarrhythmic agents9,10.
In cases of polymorphic ventricular tachycardia, magnesium sulphate is
recognized as a potential treatment option11. In cases of
ventricular arrhythmias that are refractory to initial intervention including
cardioversion and anti-arrhythmic drugs, systemic circulation can be maintained
using percutaneous cardiopulmonary bypass like portable extracorporeal membrane
oxygenation devices or ventricular-assist devices11.
CONCLUSIONS
This case highlights the prevalence of utilization of aconite
within distinct demographic groups, including monks, traditional medicine
practitioners, and local hunters. It is imperative to augment public awareness
through prominent mass media channels. Furthermore, there is an essential
requirement to promote research on the uses of aconite and foster collaborative
partnerships with the Faculty of Traditional Medicine at Khesar Gyalpo
University of Medical Sciences of Bhutan, an institution dedicated to the
training of traditional medicine practitioners in the nation.
REFERENCES
1.
World
Health Organisation (2023), World Health Statics 2023. [Full Text]
2.
Li H,
Liu L, Zhu S, Liu Q. Case reports of aconite poisoning in mainland China from
2004 to 2015: A retrospective analysis. J Forensic Leg Med. 2016 Aug;42:68–73.
[PubMed | Full Text |DOI]
3.
Tshering
U, LeVine S, Watts M. Hypotension, bradycardia and reversible conduction defect
induced by prescription of Bhutanese traditional medicines. Bhutan Health
Journal. 2018 Nov; 4(2). [Full Text | DOI]
4.
Fuchs
J, Rauber-Lüthy C, Kupferschmidt H, Kupper J, Kullak-Ublick GA, Ceschi A. Acute
plant poisoning: analysis of clinical features and circumstances of exposure. Clin
Toxicol. 2011 Aug 1;49(7):671-80. [Full Text DOI]
5.
Chen
SP, Ng SW, Poon WT, Lai CK, Ngan TM, Tse ML. et al. Aconite poisoning over 5
years: a case series in Hong Kong and lessons towards herbal safety. Drug Saf.
2012 Jul;35:575-87. [Full Text | DOI]
6.
Yeshi
K, Wangchuk P. Exploring Poisonous Plants. 1st ed. CRC Press; 2023. Chapter,
Aconitum napellus (Monkshood); p.101-12.
7.
Zhou,
W., Liu, H., Qiu, L., Yue, L., Zhang, G., Deng, H., Ni, Y., & Gao, Y.
Cardiac efficacy and toxicity of aconitine: A new frontier for the ancient
poison. Med Res Rev. 2021; 41(3), 1798–1811. [Full Text | DOI]
8.
Cho
YS, Choi HW, Chun BJ, Moon JM, Na JY. Quantitative analysis of aconitine in
body fluids in a case of aconitine poisoning. Forensic Sci Med Pathol. 2020
Jun;16(2):330-334. [PubMed | Full Text DOI]
9.
Qasem
AM, Zeng Z, Rowan MG, Blagbrough IS. Norditerpenoid alkaloids from Aconitum and
Delphinium: Structural relevance in medicine, toxicology, and metabolism. Nat
Prod Rep. 2022;39(3):460-73. [Full Text | DOI]
10.
Jesrani
G, Kaur A, Gupta M, Gupta H. Acute poisoning of aconitum: A case report and
resuscitative emergency management with amiodarone. Medical Journal of Dr. D.Y.
Patil Vidyapeeth. 2022; 15(5); 791-94. [Full Text | DOI]
11.
Coulson
JM, Caparrotta TM, Thompson JP. The management of ventricular dysrhythmia in
aconite poisoning. Clin Toxicol. 2017;55(5):313-21. [Full Text DOI]