CASE REPORT
https://doi.org/10.47811/bhj.170
Presentation of a Locally Advanced Cervical Cancer with Hydrometrocolpos: A Case Report
Namkha Dorji1,2, Sangay Tshering1,2, Nishal Chhetri 3
1Department of Obstetrics and Gynaecology, Jigme Dorji Wangchuck National Referral Hospital, Thimphu, Bhutan
2 Faculty of Postgraduate Medicine, Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan
3 Department of Pathology and Laboratory Medicine, Jigme Dorji Wangchuck National Referral Hospital, Thimphu, Bhutan
Corresponding author
Namkha Dorji
namji2002@gmail.com
ORCiD: https://orcid.org/0000-0003-3594-3159
Abstract:
Introduction: Early stages of cervical cancer remain asymptomatic. Its common symptoms are postcoital bleeding, postmenopausal bleeding, heavy menstrual flow and foul smelling blood stained discharge. Presentation of locally advanced cervical cancer with hydrometrocolpos is unusual. Case report: An 83-year-old woman who presented with a large abdomino-pelvic mass was diagnosed as benign bilateral ovarian tumour with left sided hydroureteronephrosis. During laparotomy, the mass was confirmed to be a hydrometrocolpos with left hydroureteronephrosis secondary to a locally advanced cervical cancer (FIGO IIIB). Histology confirmed the diagnosis of invasive squamous cell carcinoma of the cervix. Conclusion: Besides thorough evaluation via symptoms and signs, radiologists have an important role in guiding surgeons to the most probable diagnosis. In an elderly woman with a stenosed vagina and a pelvic mass with hydroureteronephrosis, gynecologists need to be aware of the possibility of locally advanced cervical cancer, and perform relevant preoperative assessments and plan management.
Keywords: Hydrocolpos; Hydrometra; Hydrometrocolpos; Radiation therapy; Uterine cervical cancer.
INTRODUCTION
Cervical cancer is the fourth most frequently diagnosed, and fourth leading cause of cancer death among women, with an estimated 604,000 new cases and 342,000 deaths worldwide in 20201. It is the most common cancer among women in Bhutan, with an age-standardized incidence rate of 14.4 and a mortality rate of 8.3 cases per 100,000 person-years2. The early stage of cervical cancer remains asymptomatic. When symptomatic, presentations include postcoital bleeding, intermenstrual bleeding, postmenopausal bleeding, foul smell per-vaginal discharges, pelvic pain and symptoms of distant metastasis3,4. It is incidentally diagnosed via the histological examination of total hysterectomy specimens or commonly detected by cervical cancer screening.
Herein, we report the case of an 83-year-old woman, who presented with abdominal pain and swelling, and was diagnosed as having bilateral benign ovarian tumours preoperatively. However, these pelvic masses were confirmed as hydrometra and hydrocolpos with left hydroureteronephrosis secondary to locally advanced squamous cell carcinoma (SCC) of the cervix.
CASE PRESENTATION
An 83-year-old woman developed gradual onset of lower abdominal pain and distension associated with reduced appetite and weight loss for the last two years. She didn’t report other symptoms such as vaginal discharge or postmenopausal bleeding. She had presented to different hospitals on multiple occasions, where she was managed symptomatically with oral analgesics. She is a mother of three children, all of whom were delivered vaginally at home. Her first child was delivered when she was 27 years old. Her menopause was at the age of 40 years, with no episode of postmenopausal bleeding. She is an illiterate woman who was never screened for cervical cancer. Apart from hypertension diagnosed 10 years back, she has no other medical co-morbidities. Her blood pressure is properly controlled with losartan 25 mg once daily and hydrochlorothiazide 25mg once daily.
As her pain didn’t respond to oral analgesics, she consulted a doctor at the National Referral Hospital, Thimphu. On general examination, her vitals were stable. There was no palpable lymphadenopathy in the neck, axillae and inguinal regions. Abdominal examination revealed an abdomino-pelvic lump corresponding to a 24-week gravid uterus. The lump was soft, cystic, non-tender, had free margins and was freely mobile in all four directions. Per-speculum examination revealed a stenosed upper one-third vagina with atrophied vaginal mucosa. Per-vaginal examination revealed a stenosed upper one-third part of the vagina with fullness of pelvis and difficulty in appreciating the origin of a huge lump. The cervix was not palpable in the vaginal examination.
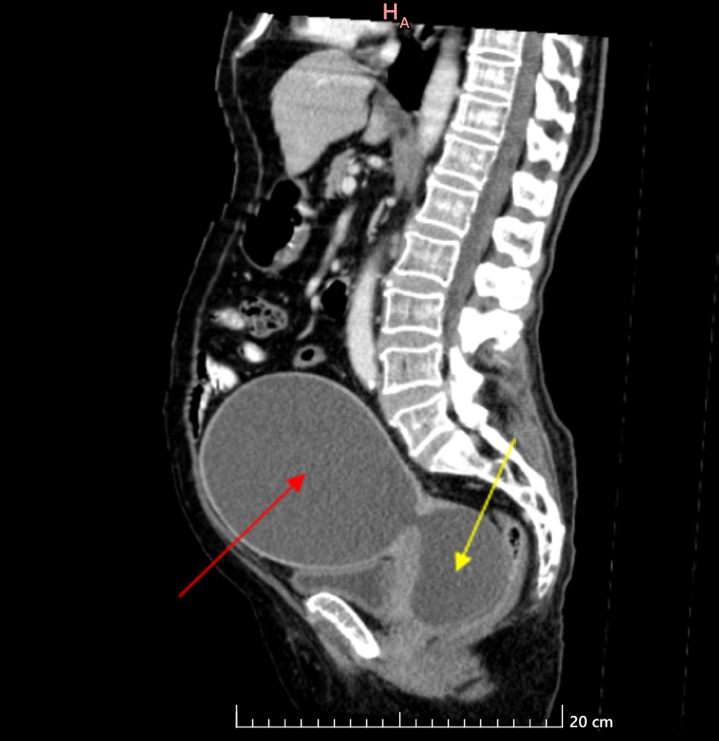
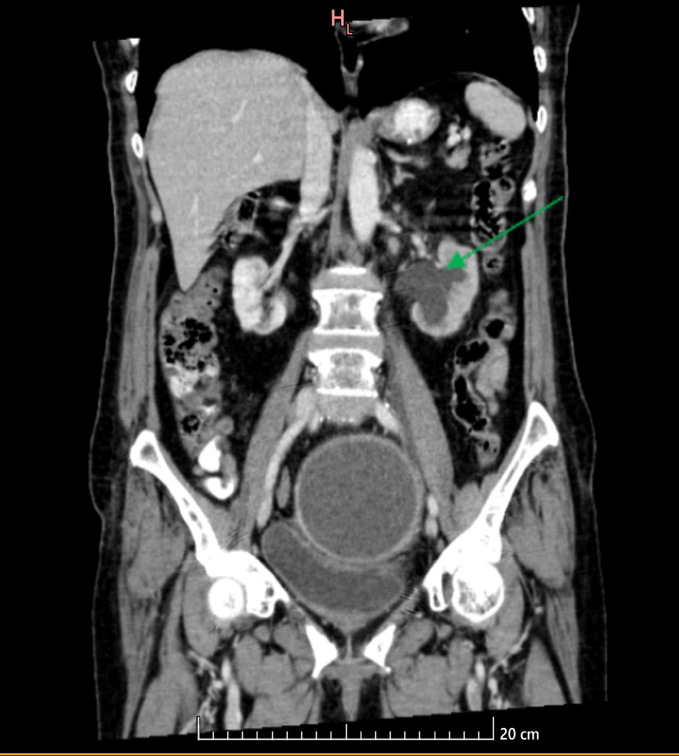
A transabdominal ultrasound scan revealed a 14x14 cm well-defined cystic lesion on the left side and another 8x7.4 cm cystic lesion with left hydroureteronephrosis. Preoperatively, CT of the pelvis detected a large right adnexal cystic lesion (13.3x12.6x11.7cm) and another cystic lesion (7.0x6.3x6.0 cm) with a resultant left sided grade 3 hydroureteronephrosis (Fig. 1a, 1b). There were no enlarged pelvic and para-aortic lymph nodes.
|
|
|
|
|
|
|
Fig. 1a: Preoperative CT that was reported as a large abdominopelvic cystic mass (13.3x12.6x11.7 cm) in continuity with a cystic lesion (7.0x6.3x6.0 cm) in the right adnexa. Cervical mass was not visible. Intraoperatively, the large cystic lesion (red arrow) was found to be hydrometra, and the smaller one (yellow arrow) was hydrocolpos. |
Fig. 1b: Preoperative CT revealing compression of the left ureter with resultant left hydroureteronephrosis (green arrow). There is mild ballooning of the renal calyces with no significant increase in the kidney size. |
|
|
|
|
Fig 2: Resected uterus in the 83-year-old woman with hydrometrocolpos secondary to locally advanced cervical cancer, showing the uterus and cervix after drainage of hydrometra. |
|
Tumor markers were normal [Carcinoembryonic antigen was 3.02 ng/ml, Alpha feto-protein was 6.95 IU/ml, Carcinoma antigen 125 was 38.98 U/ml] and serum creatinine was normal at 1.16 mg/dl.
With a preoperative diagnosis of bilateral benign ovarian tumors with normal tumor markers, an exploratory laparotomy with the intention of bilateral salpingo-oophorectomy was planned by the gynecologic oncologist.
After obtaining a written informed consent, laparotomy under general anesthesia was performed with an infra-umbilical midline incision. There was an enlarged cystic uterus corresponding to a 24-week gravid uterus with atrophied bilateral fallopian tubes and ovaries. On further exploration, another cystic lesion was noted deep in the pelvis, which was confirmed as hydrocolpos. Left hydroureteronephrosis secondary to obstruction of the distal ureter by a hard and fixed cervical mass was noted. There were no enlarged pelvic and para-aortic lymph nodes and neither were there deposits in the peritoneum, intestines, mesenteries, liver surface and under-surface of diaphragm. Intraoperatively, the patient’s daughters were informed about the possibility of locally advanced cervical cancer (FIGO IIIB), and the need for resection of distal part of left ureter with primary anastomosis of ureter with bladder.
On puncturing the distended uterus, 1000 ml of straw color fluid (hydrometra) was drained and another 500 ml was drained from the vagina (hydrocolpos). Total abdominal hysterectomy, bilateral salpingo-oophorectomy, and resection of the distal 5 cm of the left ureter was performed. The left ureter was anastomosed with the bladder with double J (DJ stent) in situ. Radical hysterectomy and pelvic node dissection were not performed, given her advanced age and the morbidity associated with combined radical hysterectomy and radiation therapy for locally advanced cervical cancer. A drain was kept in situ to monitor for the possibility of urine leak from the anastomosis. The abdomino-pelvic cavity was thoroughly irrigated with normal saline, hemostasis ensured, and the abdominal wall was closed in the standard fashion. A urethral catheter was kept in situ.
In the postoperative period, she had an uneventful recovery. Ultrasound scan of kidneys, ureters and bladder (KUB) on the 3rd postoperative day showed resolution of left hydroureteronephrosis and X-ray KUB showed that the left DJ stent was in place. The urethral catheter was removed on the 10th postoperative day, and the drain tube on the 12th postoperative day. Her wound healed well, and alternative stitches were removed on the 10th postoperative day while the remaining stitches were removed on the 12th postoperative day. She was discharged home on the 13th postoperative day on oral analgesics.
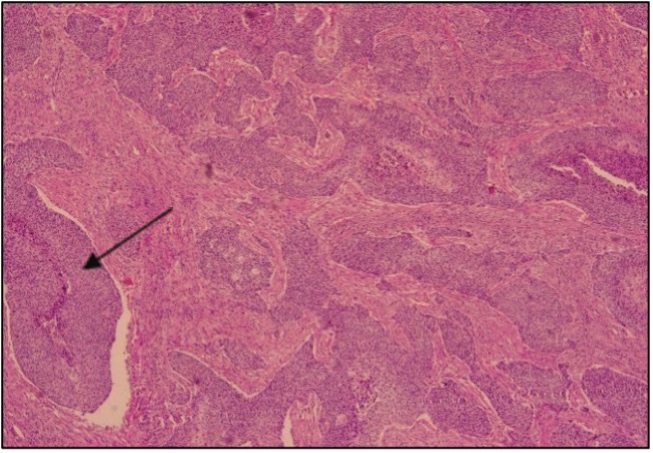
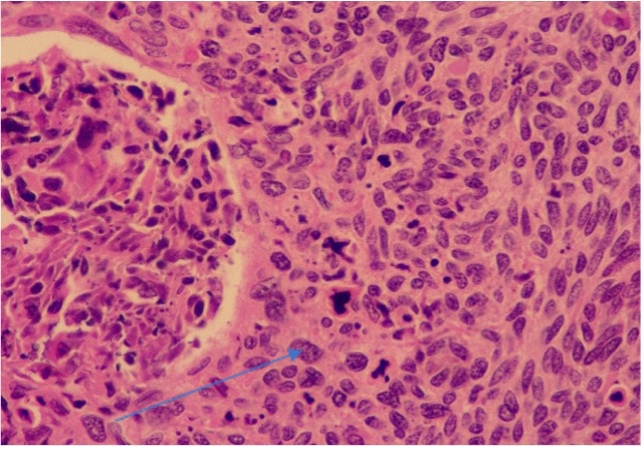
Histopathology examination confirmed SCC of the cervix (5x4cm), grade II (Fig. 3a, 3b) with deep stromal invasion with lympho-vascular space invasion (LVSI). The final diagnosis was SCC of cervix (grade II, FIGO stage IIIB) with hydroureteronephrosis.
|
|
|
|
Fig. 3a (H&E stain): Nest of squamous cells carcinoma in desmoplastic stroma, 40x (black arrow) |
Fig. 3b: Neoplastic cells with moderately pleomorphic nuclei, vesicular chromatin and occasional mitoses, 400x (blue arrow) |
On discussing adjuvant concurrent chemotherapy with external beam radiation followed by vaginal brachytherapy, the patient and family members initially decided to defer adjuvant therapy. However, on the 6th week follow up, the patient came with a positron emission tomography – computed tomography (PET-CT) report from India, which didn’t suggest any local or distant metastasis. Her wound had healed. On further discussion of adjuvant therapy, the patient party agreed for adjuvant radiotherapy (external beam radiation therapy (EBRT) 45Gy/fraction for 25 fractions over 5 weeks, followed by brachytherapy over 2-3 weeks) in India. Concurrent chemotherapy will be omitted, given her elderly age and poor performance status. The DJ stent was planned for removal 3 months after the date of surgery. After completion of radiation therapy, she would be closely monitored requiring 3 monthly follow ups for the first two years, followed by 6 monthly follow ups thereafter.
DISCUSSION
Herein, we report a case of locally advanced SCC of the cervix (FIGO IIIB) in an 83-year-old woman who was diagnosed as benign ovarian tumor preoperatively, but intraoperatively diagnosed to have a hydrometra and hydrocolpos with left hydroureter secondary to locally advanced cervical cancer.
Having presented with abdominal pain and distension, the clinical examination of abdomen was in favor of a benign abdomino-pelvic mass. CT images were reported as a bilateral ovarian cyst and tumor markers were within normal range, which led to the diagnosis of a benign ovarian tumor preoperatively. Intra-operatively, hydrometrocolpos with a large cervical growth, obliterating the left distal ureter was noted. Furthermore, there was complete adhesion of vaginal walls, which must have caused secondary hydrocolpos. She never had cervical cancer screening in her lifetime, because she was embarrassed to expose her private parts for examination by health workers. This is a common scenario in Bhutan, where a study has reported that 40.8% of its study participants were never screened for cervical cancer, and women aged <35 years or > 45 years diagnosed with cervical cancer were associated with a lack of previous screening5. The national cervical cancer screening of Bhutan recommends women between 30-65 years to be screened every 5 years with HPV-DNA test6.
There is a case report of a patient with multiple lymphadenopathies without local symptoms of cervical cancer who was diagnosed as locally advanced cervical cancer (FIGO IIB). The cervical growth was detected by 18F-Fluoro deoxy glucose (FDG) positron emission tomography/computed tomography ( 18F-FDG PET/CT) which showed focal hypermetabolic heterogeneously enhancing soft tissue mass in the uterine cervix7. An epidemiological study has reported that greater hydrometra volume (distance between the two layers of endometrium >4.75mm) is a high-risk predictive factor for uterine and cervical cancers8. However, to the best of our knowledge, there is no report of locally advanced cervical cancer that was diagnosed in a patient without any gynaecologic symptoms who presented with hydrometrocolpos.
Univariate and multivariate analysis has reported that advanced age (OR 1.11) and vaginitis (OR 3.18) are independent risk factors for hydrometra8. Inflammation is regarded as the most important cause, especially in post-menopausal women, and it is rare in premenopausal women. In our case, the hydrometra could have resulted from cervical stenosis secondary to obstruction of cervical canal by the locally advanced cervical cancer, and the hydrocolpos probably resulted from total upper vaginal stenosis secondary to vaginitis. Her age being 83 years is an independent risk factor for hydrometra.
Carcinoma of cervix that has extended to the pelvic side wall and/or hydronephrosis or non-functioning kidney (unless known to be due to another cause) is staged IIIB as per 2018 FIGO staging of the cervix uteri9. For FIGO IIIB SCC, the National Comprehensive Cancer Network recommends pelvic external beam radiation therapy (EBRT) with concurrent platinum containing chemotherapy with brachytherapy10. ESGO/ESTRO/ESP recommends EBRT with concurrent chemotherapy with image guided brachytherapy11. In our case, a simple hysterectomy with resection of distal left ureter was an intentional intra-operative decision, despite the surgeon being aware of under treatment for cervical cancer, and the disadvantages of combined treatment with surgery and radiation. The main aim was to resect the involved ureter to prevent obstructive uropathy. Primary anastomosis of ureter with bladder was performed without complications of anastomotic leakages. If FIGO IIIB cervical cancer with hydrometrocolpos was diagnosed preoperatively, the treatment would have been drainage of hydrometrocolpos and relief of left hydroureteronephrosis followed by definitive EBRT with concurrent chemotherapy, and vaginal brachytherapy.
In the postoperative period, the patient was convinved for the need of definitive treatment with radiation and chemotherapy. She was planned to undergo definitive EBRT without concurrent chemotherapy, followed by vaginal brachytherapy.
Conclusion:
In this case, hydrometrocolpos secondary to locally advanced cervical cancer was misdiagnosed as a benign ovarian tumour preoperatively. Radiologists have an important role in providing an accurate radiological diagnosis, so that proper treatment is planned. In an elderly woman presenting with abdomino-pelvic mass, with a stenosed vagina and hydroureteronephrosis, gynecologists need to be aware of the possibility of locally advanced cervical cancer and plan relevant pre-operative assessments.
Acknowledgement: We would like to thank Dr Sonam Dargay, Consultant Urologist at the Jigme Dorji Wangchuck National Referral Hospital, for his help in performing primary anastomosis of left ureter with bladder with DJ stent in situ. We are indebted to our patient, who kindly permitted us to use her de-identified clinical details and images for publication.
Consent statement: Written informed consent was obtained from the patient for her anonymized information and images to be published in this article.
REFERENCES:
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36
Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209– 49. [PubMed] [DOI]
2. Bruni L, Albero G, Serrano B, Mena M, Collado JJ, Gómez D, et al. Human Papillomavirus and Related Diseases Report. ICO/IARC Information Centre on HPV and Cancer. 2023; 296 p [Full Text]
3. Mwaka AD, Okello ES, Wabinga H, Walter FM. Symptomatic presentation with cervical cancer in Uganda : a qualitative study assessing the pathways to diagnosis in a low-income country. BMC Womens Health. 2015;15:1–13. [PubMed]
4. Aziz N, Yousfani S. Pattern of presentation of cervical carcinoma at Nuclear Institute of Medicine and Radiotherapy, Pakistan. Pak J Med Sci. 2013;29(3):814–7. [PubMed] [Full Text]
5. Baussano I, Tshomo U, Clifford GM, Tenet V, Tshokey T, Franceschi S. Cervical cancer screening program in Thimphu, Bhutan: population coverage and characteristics associated with screening attendance. BMC Womens Health. 2014;14(1):1–8. [PubMed] [Full Text] [DOI]
6. Ministry of Health. National Cervical Cancer Guidelines. Reproductive Maternal and Newborn Health Program, Department of Public Health, Ministry of Health, Royal Government of Bhutan. 2021.
7. Senthil R, Mohapatra RK, Srinivas S, Sampath MK,
Sundaraiya S. Unusual presentation of metastatic carcinoma cervix with clinically silent primary identified by 18F - flouro deoxy glucose positron emission tomography / computed tomography. Indian J Nucl Med. 2016;31(2):134– 7. [PubMed] [Full Text] [DOI]
8. Wu J, Wang S, Zhang L, Wu S. Epidemiological analysis of hydrometra and its predictive value in gynecological tumors. Front Oncol. 2022;(12):1–11. [PubMed] [Full Text] [DOI]
9. Bhatla N, Berek JS, Cuello Fredes M, Denny LA, Grenman S, Karunaratne K, et al. Revised FIGO staging for carcinoma of the cervix uteri. Int J Gynecol Obstet. 2019;145(1):129– 35. [Full Text] [DOI]
10. Abu-Rustum NR, Yashar CM, Arend R, Barber E, Bradley K, Brooks R, et al. NCCN Guidelines Insights: Cervical Cancer, Version 1.2024. J Natl Compr Canc Netw. 2023; 21 (12): 1224 - 33. [Full Text] [DOI]
11. Cibula D, Raspollini MR, Planchamp F, Centeno C, Chargari C, Felix A, et al. ESGO /ESTRO/ESP Guidelines for the management of patients with cervical cancer – Update 2023 *. Int J Gynecol Cancer. 2023;33(5):649–66. doi: 10.1136/ ijgc-2023-004429 [PubMed] [Full Text] [DOI]