ORIGINAL
ARTICLE
https://doi.org/10.47811/bhj.175
Factors affecting the level of medication adherence to
anti-diabetic treatment: A multicenter cross-sectional study in Eastern Bhutan
Tashi Wangchuk1,
Phuntsho Norbu2, Sherab Dorji2, Sonam Tashi3, Dorji
Wangmo4, Kinzang Wangdi5, Tandin Wangay6, Tshering
Norbu7
1Jigme Dorji Wangchuk National Referral Hospital
2Eastern Regional Referral Hospital
3Samdrup Jongkhar District Hospital
4Tashigang District Hospital
6Pemagatshel District Hospital
6Lhuntse District Hospital
7Tashi Yangtse District Hospital
Corresponding author:
Tashi Wangchuk
dr.tashiwangchuk2018@gmail.com
ABSTRACT
Background: Worldwide,
Diabetes Mellitus affects millions of people. It is a chronic and progressive
disease requiring a long-term treatment plan, adherence to which becomes
extremely challenging. Globally, there is a poor level of medication adherence
to anti-diabetic treatment and several studies have explored the factors
affecting medication adherence. However, in Bhutan, there is limited data on
the rate of medication adherence and factors affecting it. . Therefore, the
study aimed to find the level of anti- diabetic medication adherence and
factors affecting it. Methods: A multicenter cross-sectional
observational study was conducted involving six eastern district hospitals from
June 2019 to February 2020. Research participants were randomly selected from
the daily cohort of patients visiting diabetic clinics. Results: Amongst
the 390 participants, the overall level of adherence reported in this study was
intermediate with a mean Morisky Medication Adherence Scale 8 Items (MMAS-8)
score of 6.06 (95% CI 5.91-6.22). Nearly 40% demonstrated a low level of
adherence (MMAS-8 score <6). There was a statistically significant
(p<0.05) association between mean MMAS-8 scores and adverse drug reactions,
the drug regimen (polypharmacy or monotherapy) and the type of diabetes
mellitus. Conclusion: This study revealed an intermediate level of
medication adherence to anti-diabetic treatment in the eastern region of
Bhutan. Adverse drug reactions and polypharmacy resulted in a lower level of
adherence. However, further studies are needed to draw a definitive conclusion.
Keywords: Adherence level; Bhutan;
Diabetes Mellitus; Morisky; Risk factors.
INTRODUCTION
Diabetes Mellitus (DM) is a chronic
and progressive disease with a global prevalence of 10.5% (536.60 million
people) in 20211. Over the past few decades, the number of diabetic
patients has risen faster in low and middle-income countries. Bhutan reported
an incidence of 75-82 persons per 10,000 people in 20202.
Non adherence to medication is a
major concern for all chronic diseases requiring life-long treatment3.
Medication adherence is the extent to which a patient gets treatment in
accordance with the prescribed interval and dose4. Though it is a
global concern, medication adherence is generally considered poor worldwide,
with minimal importance accorded to it even during hospital consultations5,6.
Although Bhutan shares concerns on
the low level of medication adherence to chronic diseases and its related
consequences, there are no studies examining the level of medication
adherence. With this lack of data, health consequences due to nonadherence to
prescribed treatment could be significant. In order to address this knowledge
gap, this study intended to study the level of adherence and risk factors
affecting antidiabetic treatment in eastern region of Bhutan.
METHODS
The study was a multicenter
cross-sectional observational study conducted in six district hospitals in
eastern Bhutan. It was conducted from June 2019 to February 2020.
Study population and sampling technique
Diabetic patients (both DM type 1 and
2) above the age of 18 years visiting the diabetic clinics of the 6 eastern
hospitals were eligible participants. Those with gestational DM and mentally
challenged patients without a capacity to consent were excluded from the
study. A simple randomization technique was used for recruiting participants,
wherein every third or fifth diabetic patient visiting the diabetic clinic who
fulfilled the inclusion criteria were approached for inclusion into the study.
They were enrolled after receiving informed written consent.
The sample size was calculated based
on an estimated total number of patients with DM in Bhutan of 15,000 in the
year 2019 and a non-adherence rate of 50% to the treatment. A minimum sample
size of 375 was calculated, considering a 95% confidence interval with a margin
of error of 5%. To offset loss of subjects through refusal to consent or
incomplete data, we took a sample size of 400.
Data collection
Data was collected by focal persons
of DM clinic working in the six identified hospitals. Some of these hospitals
operate diabetic clinics daily whereas others operate two to three days a week.
Each recruited participant was provided with information about the research and
consent for participation was obtained. The diabetic clinic’s focal person
collected relevant data by reading out questions from a structured
questionnaire.
The questionnaire
consisted of socio demographic details, details about the type of DM, type of
treatment regimen (mono or polytherapy), route of administration of
medications, history of any adverse drug reactions, presence of any other
comorbidity, and the time taken to reach the nearest health facility. The
Morisky Medication Adherence Scale 8 Items (MMAS-8) was also a part of the
questionnaire, to determine the level of adherence. The MMAS-8 is a tool which
has been tested and validated in many languages for chronic diseases requiring
long term treatment7-9. The owner of the tool granted us the
permission to use the tool via certificate Number: 1207-2004-207-31418477.
MMAS-8 consists of 8 closed-ended questions.
Except for item number 8, all other questions are responded with either Yes or
No. Each ‘Yes’ response is accorded a score of ‘0’ while each ‘No’ response is
accorded a score of 1, except for item 5, where ‘Yes’ response is scored 1 and
‘No’ response is scored 0. Item number 8 includes a 5-point Likert response
(0-4), corresponding to scores of 0, 0.25, 0.50, 0.75, and 1, respectively. As
per the MMAS-8 score, the level of medication adherence can be high (=8), intermediate
(6 & 7) or low (< 6)7.
Statistical analysis
For descriptive analysis of continuous variables, mean and SD
were employed and for categorical variables, percentages were used. For
inferential analysis, Chi-square test was used. Statistical analysis was
conducted using EpiData Software Version 3.1. The primary outcome of this study
was to find the level of adherence to anti-diabetic medications, and were
reported as being low, intermediate or high.
Ethical clearance
For this study, ethical approval was
accorded by the Research Ethics Board for Health, Ministry of Health, Bhutan
(Ref. No. REBH/Approval/2019/022 23/06/ 2019 dated 23/06/ 2019).
RESULTS
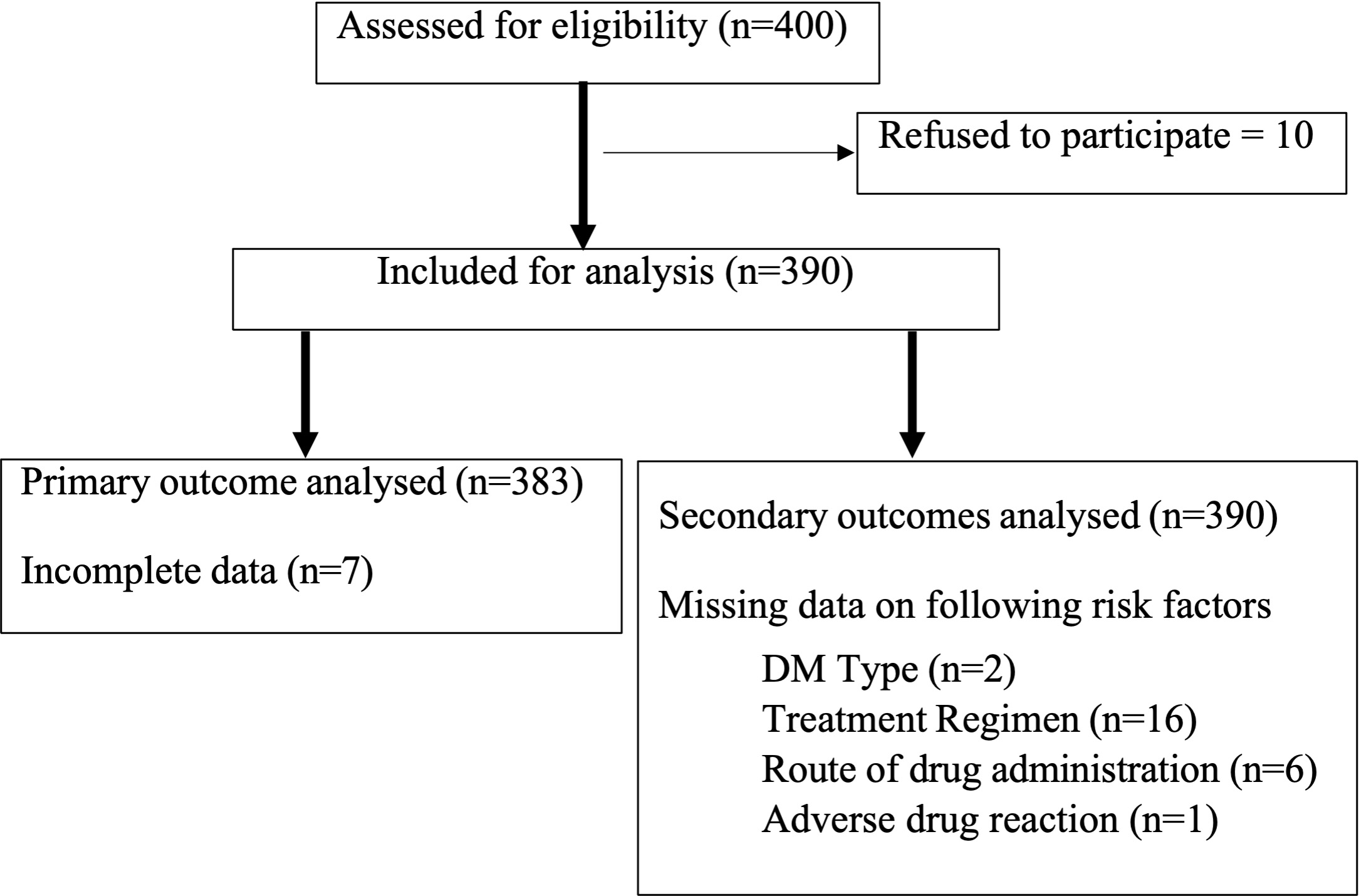
Of the 400 participants recruited, 390 were included in the
analysis. To analyse the primary outcome of level of medication adherence, only
383 were included since 7 had missing data. Figure 1 depicts the process of
patient recruitment and analysis.
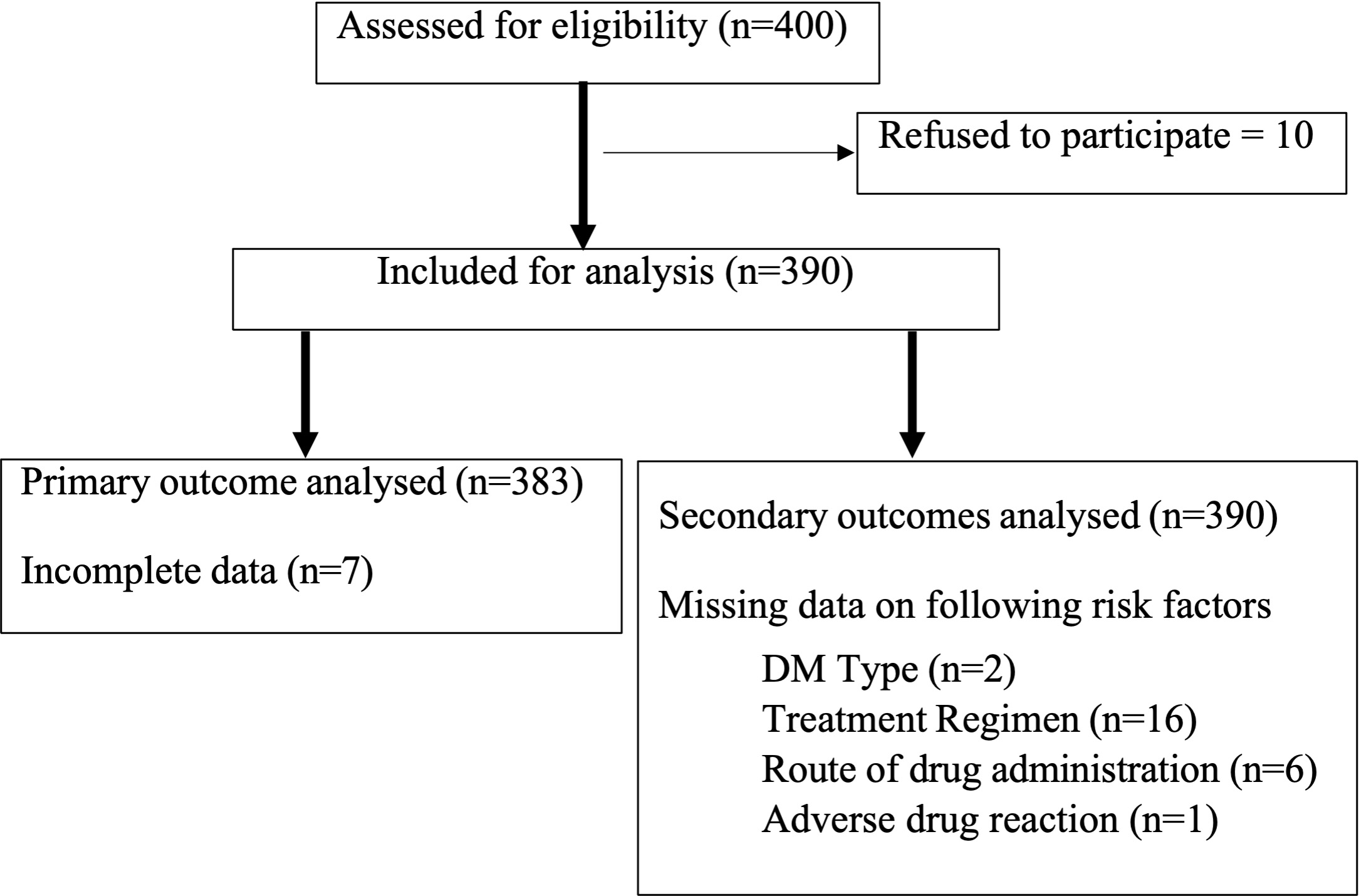
Figure 1. Flow diagram depicting the process of
recruitment of participants in the six eastern district hospitals of Bhutan,
June 2019-February 2020
The majority of the participants in this study (49.20%) were
availing services from the Eastern Regional Referral Hospital (ERRH). Females
outnumbered males (54.4% vs. 45.6%) and participants in the age group of 51-65
years constituted the majority (161, 41.3%). As depicted in Table 1, patients
with Type 2 DM (378, 97.4%) outnumbered those with Type 1 DM and a majority of
them (257, 65.90%) had an additional co-morbidity. Most of the participants
(361, 94%) were on oral hypoglycemic agents and most did not report
experiencing an adverse effect to treatment (314, 80.70%).
The overall mean MMAS-8 score was
6.06 (95% CI 5.91-6.22). Amongst the 383 participants included in the analysis
of the primary outcome, 16.40% (n=63) reported high level of adherence, 41.30%
(n=158) reported intermediate level of adherence and 42.30% (n=162) reported a
low level of adherence.
Table
1. Baseline characteristics of participants in the six eastern hospitals of
Bhutan, June 2019-February 2020, n=390
|
Variables
|
N (%)
|
|
Sex
Male
Female
|
178 (45.6)
212 (54.4)
|
|
Age group
<35 years
old
35-50 years
old
51-65 years
old
>65 years
old
|
13 (3.30)
122 (31.30)
161 (41.30)
94 (24.10)
|
|
Education level
Illiterate
Literate
|
287 (73.60)
103 (26.40)
|
|
Occupation
Employed
Retired
Farmer
Housewife
|
86 (22.10)
29 (7.40)
177 (45.40)
98 (25.10)
|
|
Type of DM
DM Type 1
DM Type 2
Missing data
|
10 (2.60)
378 (96.90)
2 (0.50)
|
|
Co-morbidity
Yes
No
|
257 (65.90)
133 (34.10)
|
|
Treatment Regimen
Monotherapy
Polytherapy
Missing data
|
185 (47.40)
189 (48.50)
16 (4.10)
|
|
Route of administration
Oral
Injection
Both oral and
injection
Missing data
|
361 (92.60)
7 (1.80)
16 (4.10)
6 (1.50)
|
|
Adverse drug reaction
Yes
No
Missing data
|
75 (19.20)
314 (80.50)
1 (0.30)
|
|
Hospitals
Eastern Regional Referral
Hospital
Trashigang District Hospital
Pemagatshel District Hospital
Samdrup Jongkhar District
Hospital
Lhuentse District Hospital
Trashi Yangtse District
Hospital
|
192 (49.20)
62 (15.90)
48 (12.30)
50 (12.80)
16 (4.10)
22 (5.60)
|
|
Average time taken to reach health facility
<1 hour
1-3 hours
>3 hours
|
191 (49.00)
179 (45.90)
20 (5.10)
|
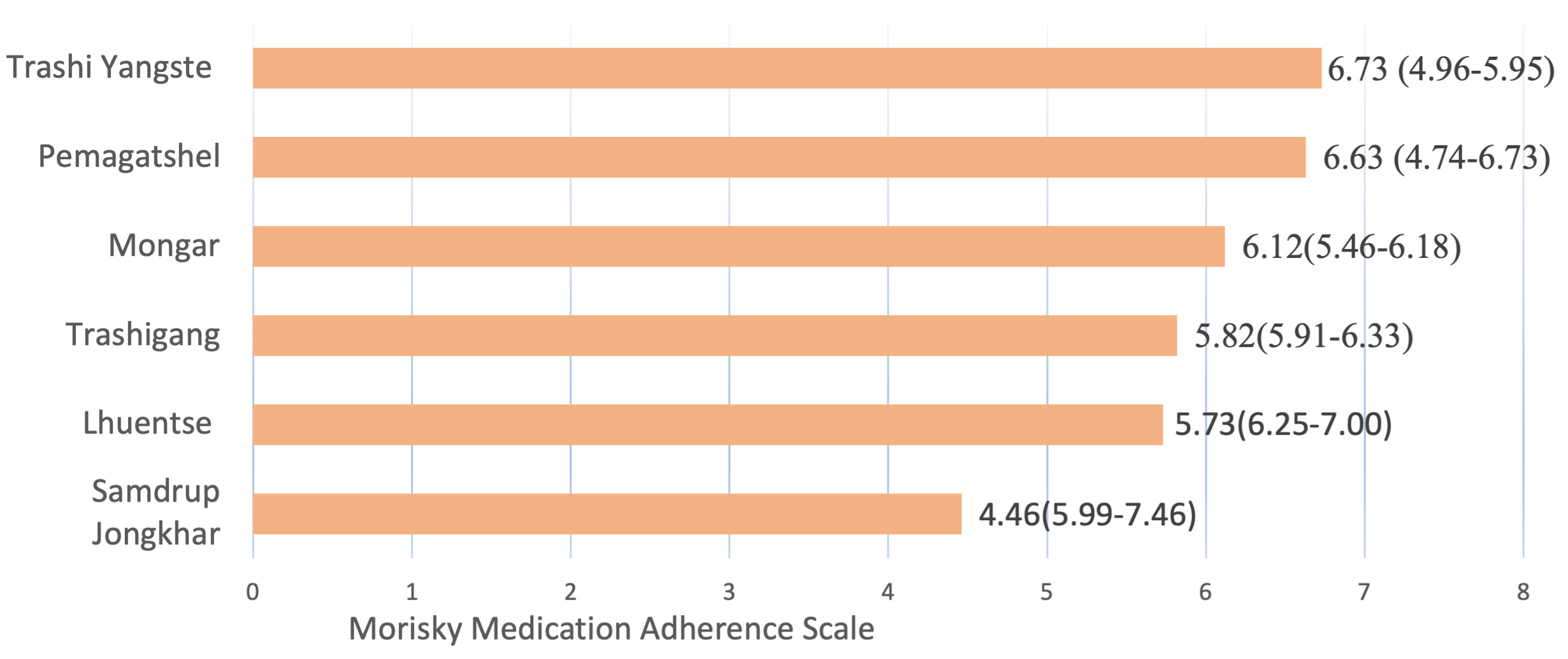
Patients availing DM
treatment at Samdrup Jongkhar district hospital reported the lowest mean MMAS-8
score of 4.46 while patients availing DM treatment at Trashi Yangtse district
hospital reported the highest mean MMAS-8 scores of 6.73. The mean scores of
patients from other hospitals ranged from 5.73 to 6.63 as reflected in Figure
2.
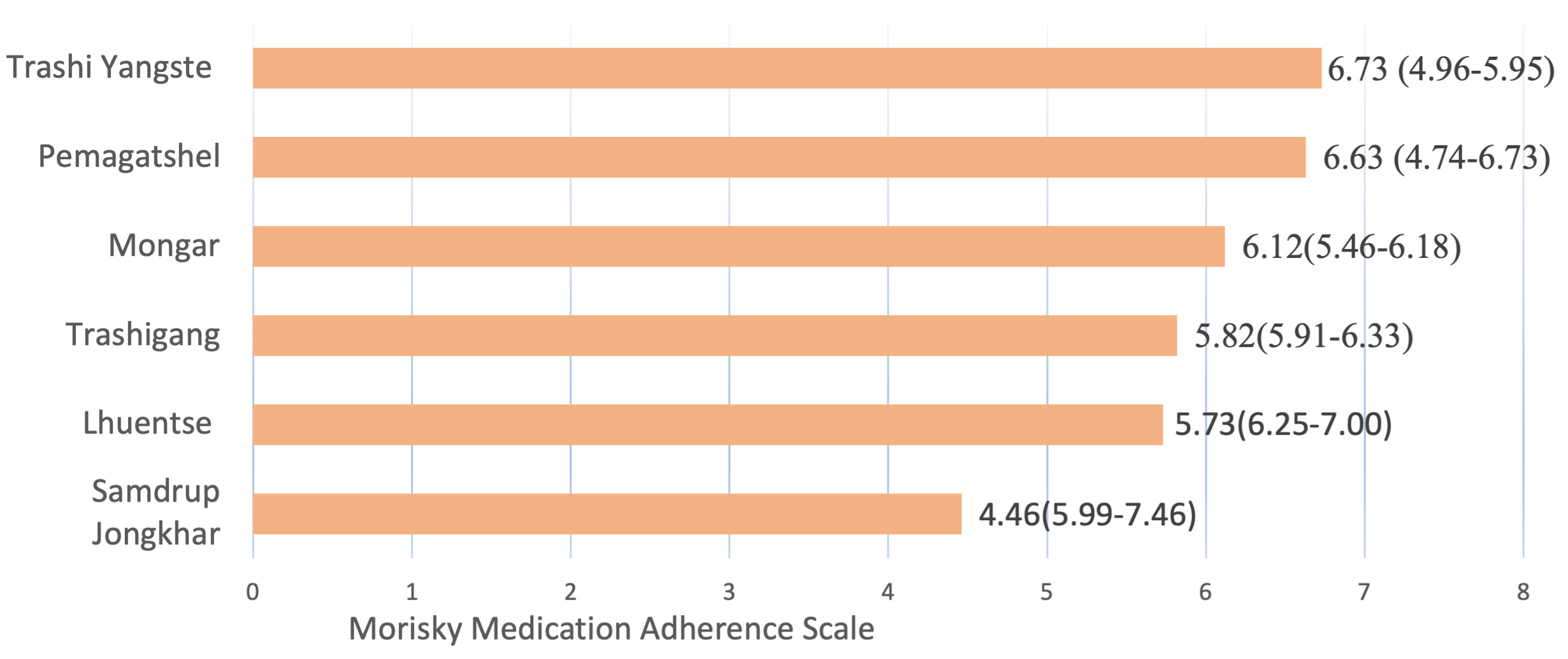
Figure 2. Bar graph
depicting mean MMAS-8 score in 6 hospitals of Bhutan. [The numbers at the end of
bar represent means scores with 95% confidence intervals within brackets.]
Adverse reactions to anti-diabetic drugs, types of treatment
regimen (polypharmacy or monotherapy) and the type of DM demonstrated a
statistically significant (p<0.05) association with mean MMAS-8 score, as
shown in Table 2.
Table 2. Risk factors affecting the
medication adherence amongst diabetic patients availing services at six eastern
hospitals of Bhutan, June 2019-February 2020, n=390
|
Risk factors
|
Adherence scores
|
p-value
|
|
Mean score
|
95% CI
|
|
Age group
<30 years
35 – 50 years
51 – 65 years
>65 years
|
6.25
5.93
6.04
6.26
|
5.36 – 7.14
5.66 – 6.19
5.78 – 6.30
5.96 – 6.55
|
0.46
|
|
Sex
Male
Female
|
6.01
6.10
|
5.78 – 6.24
5.88 – 6.31
|
0.58
|
|
Marital status
Married
Unmarried
|
6.05
6.21
|
5.89 – 6.21
5.61 – 6.82
|
0.59
|
|
Level of education
Literate
Illiterate
|
6.08
6.04
|
5.90 – 6.26
5.72 – 6.36
|
0.82
|
|
Occupation
Employed
Retired
Farmer
Housewife
|
5.97
6.22
5.92
6.22
|
5.63 – 6.31
5.52 – 6.93
5.70 – 6.14
6.00 – 6.63
|
0.21
|
|
Treatment regimen
Monotherapy
Polytherapy
|
6.28
5.84
|
6.06 – 6.49
5.62 – 6.06
|
0.00
|
|
Types of diabetes mellitus
Type 1
Type 2
|
4.95
6.09
|
3.84 – 6.06
5.94 – 6.25
|
0.02
|
|
Route of drug administration
Oral
Injection
Both
|
6.08
4.93
6.02
|
5.92 – 6.24
2.83 – 7.03
5.28 – 6/75
|
0.14
|
|
Presence of co-morbidities
Yes
No
|
6.17
5.86
|
5.98 – 6.35
5.58 – 6.14
|
0.06
|
|
Average travel time to nearest
health facility
|
|
<1 hour
1 – 3 hours
>3 hours
|
6.13
6.00
6.05
|
5.90 – 6.36
5.78 – 6.22
5.27 – 6.83
|
0.74
|
|
Are you informed on the
need to take medicines / injection if you don’t feel any symptoms?
|
|
Yes
No
|
6.02
6.35
|
5.86 – 6.18
5.81 – 6.89
|
0.05 (One-way ANNOVA)
|
|
Do you know why you are taking
medications?
|
|
Yes
No
|
6.10
5.64
|
5.95 – 6.26
5.04 – 6.24
|
0.10
|
DISCUSSION
With an overall mean MMAS-8 score of
6.06, this study reports an intermediate level of adherence to oral
anti-diabetic drugs amongst diabetic patients availing services from six
hospitals in the eastern part of Bhutan. However, 42% of participants reported
a low level of medication adherence, which is concerning. This rate is similar
to the global adherence rate of below 50%6,10,11. Even developed
countries like the USA have reported that 40% of patients with Type 2 DM are
nonadherent, the United Kingdom reports that 39.9% were nonadherent, and China
reports a non-adherence rate of 54.6% amongst diabetic patients7,12,13.
However, our neighboring country India has reported a lower non-adherence rate
of 25.5% amongst diabetic patients availing services from 3 government
hospitals in Delhi8.The studies in the United Kingdom and China only
assessed adherence to oral diabetic agents and excluded those using insulin.
Low level of medication adherence amongst
diabetic patients is associated with poor glycemic control, diabetic micro and
macro vascular complications, and eventual increased morbidity and mortality12.
In the long run, it not only affects physical health of the patients but also
becomes a financial burden to a country9,13.
While comparing mean
MMAS-8 scores among diabetic patients availing services from the 6 eastern
hospitals, the current study noted that participants from Samdrup Jongkhar
district reported the lowest level of adherence whereas participants from
Trashi Yangtse district revealed the highest level of adherence. Samdrup
Jongkhar has only 7 primary health care centers, 3 subpost facilities and 1
district hospital to cater to its population of 35,079. Except for one
additional sub-post, the number of healthcare facilities have remained the same
since 201814,15. This could be a potential reason why they had the
lowest adherence. However, disproportionate sampling from the various hospitals
could have impacted the mean adherence rates. A study in rural Kerala in India
reported poor adherence in 74% of diabetic patients using the MMAS-8 tool16.
Rural areas usually have poor socio-economic conditions which may influence the
adherence level.
Higher levels of education
have been reported to bring about a positive influence on medication adherence10,12.
However, findings of our study did not reveal a significant association of
level of education with medication adherence levels. This may be because health
advocacy programs are regularly conducted in local languages by health
assistants in the primary health care centers in Bhutan. Thus, the level of
formal schooling may have limited influence on the understanding of being
adherent to medications.
This study, however,
demonstrated a significant association between mean MMAS-8 score and
polypharmacy. A similar finding was also revealed in other studies where
multiple drug regimens were associated with reduced levels of medication
adherence9,10. The need to take multiple drugs make the treatment
complex with a potential for forgetting a few doses16,17. An adverse
event with the medication has been reported to adversely affect medication
adherence18. This study noted a statistically significant association
between a past episode of adverse drug reaction and the level of medication
adherence.
The strength of this study is that it
was conducted in a free healthcare setting involving 6 district hospitals of
eastern Bhutan, which represents 24% of Bhutanese population19.
However, the authors also admit to have few limitations. The study experienced
a few dropouts due to incomplete data and the sample size was not proportionate
among the districts.
CONCLUSION
An intermediate level of adherence to oral and injectable
antidiabetic medicine is noted amongst diabetic patients in the eastern region
of Bhutan. While it is premature to draw any conclusion with just one study,
this sets the stage to conduct other studies to address factors resulting in
nonadherence to medications.
ACKNOWLEDGEMENTS
We express our gratitude to Mr.
Thinley Wangdi who provided constant assistance in developing this manuscript.
We would also like to thank all our patients for consenting to participate in
the study.
REFERENCES
1.
Sun H,
Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes
Atlas: Global, regional and country-level diabetes prevalence estimates for
2021 and projections for 2045. Diabetes Res Clin Pract. 2022; 183:109119. [PubMed] [Full Text] [DOI]
2.
Ministry
of Health: Annual Health Bulletin 2020. Thimphu: Health Management and
Information System, Policy & Planning Division, Ministry of Health, Royal
Government of Bhutan; 2020; 107.p [Full Text]
3.
Rombopoulos
G, Hatzikou M, Athanasiadis A, Elisaf M. Treatment compliance with fixed-dose
combination of vildagliptin/metformin in patients with type 2 diabetes mellitus
inadequately controlled with metformin monotherapy: a 24-week observational
study. Int J Endocrinol. 2015; 2015:251485 [PubMed] [Full Text] [DOI]
4.
Raum
E, Krämer HU, Rüter G, Rothenbacher D, Rujosemann T, Szecsenyi J, et al.
Medication non-adherence and poor glycaemic control in patients with type 2
diabetes mellitus. Diabetes Res Clin Prac. 2012; 97(3):377-84. [PubMed] [Full Text] [DOI]
5.
Barnett
NL. Medication adherence: where are we now? A UK perspective. Eur J Hosp Pharm.
2014;21:181-4. [Full Text] [DOI]
6.
Iglay
K, Cartier SE, Rosen VM, Zarotsky V, Rajpathak SN, Radican L, et al.
Meta-analysis of studies examining medication adherence, persistence, and
discontinuation of oral antihyperglycemic agents in type 2 diabetes. Curr Med
Res Opin. 2015;31(7):1283-96. [Full Text] [DOI]
7.
Wu P,
Liu N. Association between patients’ beliefs and oral antidiabetic medication
adherence in a Chinese type 2 diabetic population. Patient Prefer Adherence.
2016; 10:1161-7. [PubMed] [Full Text] [DOI]
8.
Basu
S, Khobragade M, Kumar A, Raut DK. Medical adherence and its predictors in
diabetes mellitus patients attending government hospitals in the Indian
capital, Delhi, 2013: A cross-sectional study. Int J Diabetes Dev Ctries.
2015;35(2):95-101 [Full Text] [DOI]
9.
Odegard
PS, Gray SL. Barriers to medication adherence in poorly controlled diabetes
mellitus. Diabetes Educ. 2008;34(4):692-7. [Full Text] [DOI]
10.
Cramer
JA. A Systematic Review of Adherence With. Diabetes Care. 2004; 27(5):1218–24.
[Full Text] [DOI]
11.
World
Health Organization. Adherence to long-term therapies: evidence for
action.Geneva, World Health Organization. 2003. 196 p. [Full Text]
12.
Samu
AM, Amirthalingam PS, Mohammed OS. Assessment of patient medication adherence
among the type 2 diabetes mellitus population with peripheral diabetic
neuropathy in South India. J Taibah Univ Med Sci. 2017;12(2):164–8. [PubMed] [Full Text] [DOI]
13.
Tunceli
K, Iglay K, Zhao C, Brodovicz KG, Radican L. Factors associated with adherence
to oral antihyperglycemic monotherapy in patients with type 2 diabetes mellitus
in the United Kingdom. Diabetes Res Clin Pract. 2015;109(3):e27–31.[Full Text] [DOI]
14.
Ministry
of Health. Annual Health Bulletin 2019.Thimphu; Health Management and
Information System, Policy & Planning Division, Ministry of Health, Royal
Government of Bhutan;2019; 109p. [Full Text]
15.
Ministry
of Health. Annual Health Bulletin 2023. Thimphu; Health Management and
Information System, Policy & Planning Division, Ministry of Health, Royal
Government of Bhutan; 2023; 171p. [Full Text]
16.
Sankar
UV, Lipska K, Mini GK, Sarma PS, Thankappan KR. The adherence to medications in
diabetic patients in rural Kerala, India. Asia Pac J Public Health. 2015;
27(2):NP513-
23. [Full Text] [DOI]
17.
Karla
S, Das AK, Priya G, Ghost S, Mehrotra RN, Das S, et al. Fixed-dose combination
in management of type 2 diabetes mellitus: Expert opinion from an international
panel. J Family Med Prim Care. 2020;9(11):5450–7. [Full Text] [DOI]
18.
Leporini
C, De Sarro G, Russo E. Adherence to therapy and adverse drug reactions: is
there a link? Expert Opin Drug Saf. 2014;13 Suppl 1:S41-55. [Full Text] [DOI]
19.
National
Statistics Bureau. Population 2017. National Statistics Bureau. [Full Text]
AUTHORS CONTRIBUTION
TW: Concept, design, data collection and analysis, manuscript
writing &review
PN: Concept, design, data collection and analysis, manuscript
writing & review
SD: Concept, design, data collection & review
ST: Concept, design, data collection & review
DW: Concept, design, data collection & review
KW: Concept, design, data collection & review
TW: Concept, design, data collection & review
TN: Concept, design, data collection & review
Authors agree to be accountable for all respects of the work in ensuring
that questions related to the accuracy and integrity of any part of the work
are appropriately investigated and resolved.
CONFLICT OF INTEREST
None
GRANT SUPPORT AND FINANCIAL DISCLOSURE
None