INTRODUCTION
Cardiovascular disease (CVD) is a growing health problem and a major contributor to the epidemic of chronic diseases1. It encompasses coronary heart disease, stroke, peripheral arterial disease, rheumatic and congenital heart disease, and deep vein thrombosis1. In 2017, CVD was the biggest contributor to the total burden of disease2. CVDs also led to the highest age standardized death rate (ASDR), with coronary artery diseases and stroke being the primary contributors.
Epidemiological transition to NCD and the rise of CVD The disease epidemiology has transitioned from communicable to non-communicable diseases (NCD) over the past two decades, with CVDs being one of the leading contributors. This transition has led to an estimated 17.8 million deaths worldwide due to CVD, with 80% of them occurring in low- and middle-income countries (LMIC)3. Furthermore, congenital heart diseases (CHD) and rheumatic heart disease (RHD) have a looming presence in LMICs, contributing significantly to heart failure and death4. A plausible reason for this high occurrence is the limited capacity and resources in LMICs which results in late detection and thus, growing adult congenital heart disease burden5-9. Despite CVD accounting for 30% of all-cause mortality in the Southeast Asia region in 2021, access to cardiac surgical services is limited, especially in LMICs10,11.
Bhutan is no different in terms of the epidemiological transition to NCDs. With CVD contributing to 18.4% of Bhutan’s total disease burden 24 years ago, ischemic heart disease has caused 64.6 deaths per 100,000 population in 202112. Figure 1 reflects the drastic increase in the prevalence of noncommunicable diseases, majority of which are risk factors for CVD13. In fact, hypertension, diabetes mellitus, ischemic heart disease, and rheumatic heart disease combined have surpassed all other selected non-communicable diseases combined in Bhutan14.
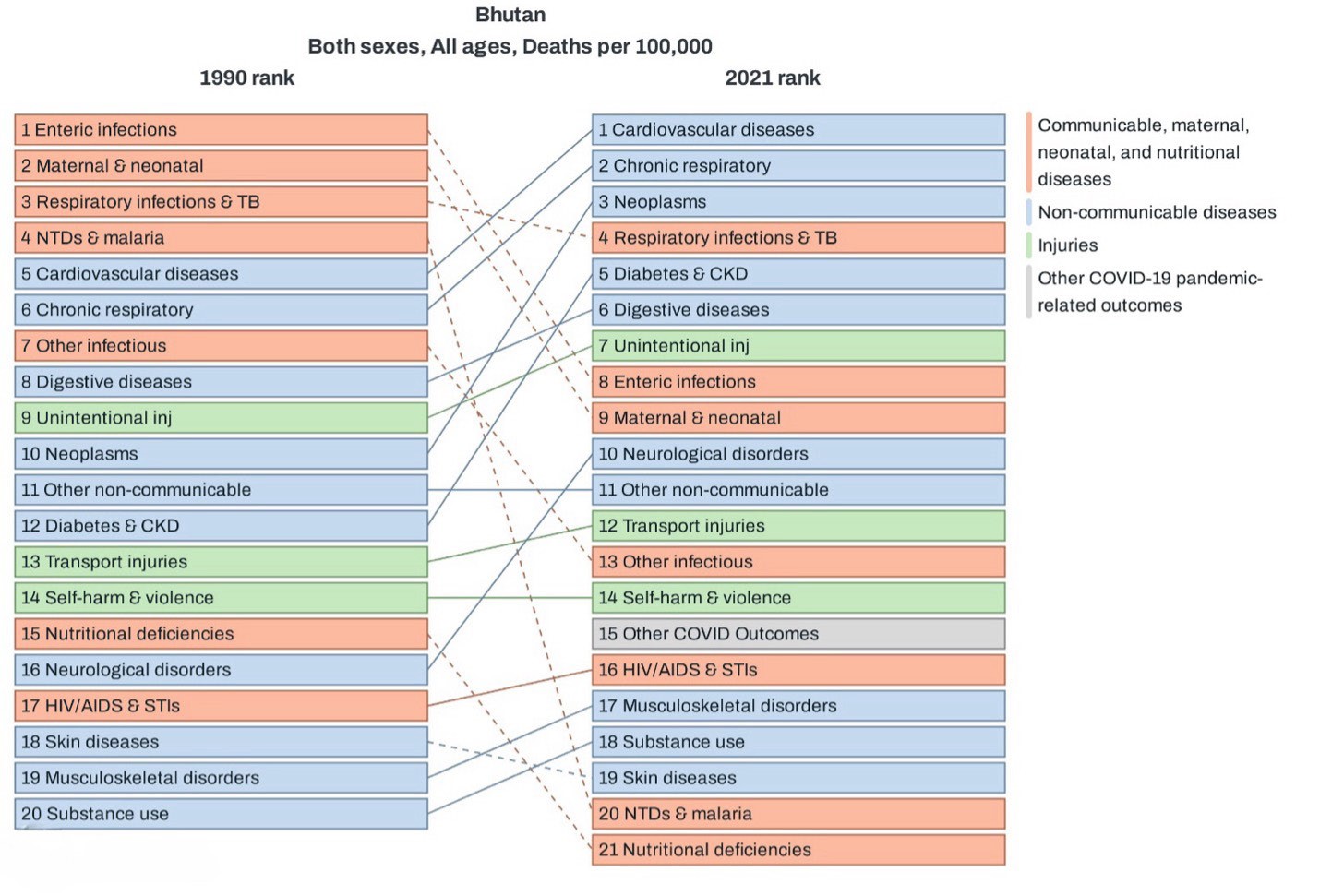
Fig 1. Comparison of Bhutan’s burden of disease between 1990 and 202113.
Cardiovascular disease burden and its risk factors in Bhutan
This growing burden of risk factors for CVD has had significant morbidity, mortality and economic impacts. Data from the World Heart Observatory reveal that the crude CVD mortality is 160 per 100,000 population with an age-standardized CVD mortality of 247 per 100,000 population, and age-standardized CVD incidence of 698 per 100,000 population3. Data from a study in the eastern regional referral hospital in Bhutan reported the incidence of CHD in their center as 68 per 1000 live births, which is much higher compared to the global incidence of 8-50 per 1000 live births14-16.
These numbers are expected to rise because the risk factors for CVD including hypertension and diabetes mellitus, have been on a steady rise as depicted in Figure 217. The National Health Survey in 2023 revealed that the 1.8% of Bhutanese aged 40-69 years have a ≥30% 10-year CVD risk17. Furthermore, the overall prevalence of smoking is 10% and more than 40% of the population is obese, both modifiable risk factors for CVD18,19.
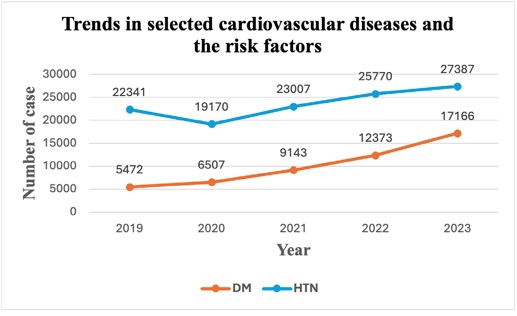
Fig 2. Trend of hypertension and diabetes mellitus, common risk factors of CVD. HTN: hypertension, DM: Diabetes Mellitus17
Current state of cardiovascular services in Bhutan
With the catheterization laboratory, the intervention cardiologist treats coronary artery disease with stents and patent ductus arteriosus and atrial septal defects with device closure devices. However, an open-heart surgery facility is essential to manage complex cases that cannot be treated with minimally invasive interventions. Without surgical facilities, costly referrals abroad will continue. The constitution of Bhutan mandates free access to basic public health services, but in practice, healthcare remains free at all levels, including advanced surgical interventions and referrals abroad20.
Bhutan’s three-tiered health care system has primary healthcare at the cornerstone translating to remarkable progress in health indicators like maternal mortality rate, infant mortality rate and immunization coverage18. Despite the success achieved in primary healthcare, access to cardiac surgical services remains a critical gap. Bridging this gap is very important at this juncture when CVD ranks first in the top 10 cause of death in 202312.
Bhutan faces a critical shortage of healthcare professionals, with a doctor-to-population ratio of 4.6:10000, far below the WHO’s recommendation of 1:1000 population21,22. Furthermore, the cardiologist and cardiac surgeon ratios stand at 1:385138 and 1:770276, respectively, making cardiovascular care delivery challenging23. Nurse shortages further exacerbate the issue, with a nurse to population ratio of 20.9:10000, likely worsened by the recent attrition24. Urgent policy intervention is needed to retain healthcare workers and strengthen specialized services.
Bhutan’s free health care system places over 70% of the annual current health expenditure on the government, with approximately 40% spent on non-communicable diseases, including CVD25. This indicates the growing burden of the CVD in Bhutan as well as the government’s commitment to address it26. Bhutan's total health expenditure as a share of GDP has remained around 4% over the recent years25-27. However, funding specialized cardiac surgeries remains a challenge, especially when many CVD patients require referral to India. Between 2021 and 2023 alone, 1.24 billion ngultrums were spent for outcountry patient referrals, of which nearly a quarter was spent on 506 referred CVD patients28. In addition to the treatment cost, the government also bears the cost for travel and daily living for both the patient and the caregiver.
Even for the free services provided by the catheterization laboratory, hidden costs and out-of-pocket payments remain, especially for patients residing in remote areas who have to bear high transport and accommodation costs22,25. While Bhutan has one of the lowest out of pocket expenditures (OOP) as a percentage of its total health expenditure in South Asia, financial barriers do persist22. This highlights the importance of ensuring accessibility when introducing specialized healthcare services to prevent disproportionate financial burdens to those in need. The establishment of Bhutan’s first cardiac catheterization laboratory operated by the only interventional cardiologist, was a significant milestone in combating CVD. It immediately reduced monthly referrals to India from 20 to 4, saving nearly 50 million ngultrums in revenue29,30. This success underscores the need for more specialized services within Bhutan.
While the cardiac catheterization laboratory is a significant achievement, disparities remain. North America has one such center per 120,000 population, while Europe and Australia have one per million population, highlighting the disparity in the distribution of cardiac surgical services4. This imbalance is alarming, considering CVDs are the main cause of disability and death in LMICs11,31,32.
Globally, there is one cardiovascular and thoracic (CVT) surgeon per 0.61 million people, but in Asia, it is 1 per 25 million11. Bhutan, with one cardiac surgeon for 0.7 million, fares better, provided cardiac surgical services are fully operational.
Challenges and way forward
Bhutan is making gradual progress in cardiac surgical care, with one interventional cardiologist and a cardiothoracic surgeon providing specialized cardiac interventions, and a technician training in perfusion technology abroad. The procurement of cardiac surgical equipment is in progress and the recently established surgical intensive care unit at the national referral hospital will enhance its capacity to manage cardiac cases. These developments are important strides towards establishing comprehensive cardiac surgical services in the country.
Despite the high initial cost, cardiac surgery services will have significant long-term benefits, given Bhutan’s 70% rise in the all-age mortality rate from CVD, the highest amongst neighboring countries33. Establishing a comprehensive cardiac surgical center is challenging but is feasible with support from the government, partners and non-governmental organizations34,35. With the gradual withdrawal of external donors owing to Bhutan’s graduation from the LDC category, innovative health financing strategies are needed to fund training and equipment for cardiac surgery services. Partnering with overseas experts for training, skill transfer and technical support, as seen in other developing countries, can accelerate progress36. With key infrastructure and human resources such as operation theatre, intervention cardiologist, and intensivist already in place, leveraging on these will minimize cost and time.
Skilled human resources are essential for successful cardiac surgery services. Urgent recruitment of key personnel including cardiac anesthesiologist, specialized scrub nurses, critical care and rehabilitation teams is needed (Table 1). With Bhutan’s own medical college increasing the pool of medical doctors, this is apt time to develop a sustainable human resource plan for sustainable cardiac services37. Without a concrete plan, Bhutan risks missing the third sustainable development goal of reducing premature NCD deaths by one-third by 20304.
Table 1. Existing requirement to meet the minimal standards of human resources and equipment to initiate open heart surgery in Bhutan
|
Requirement |
Number |
|
Additional cardiac surgeon |
1 |
|
Perfusionists |
2 |
|
Intensive care unit (ICU) beds |
2 |
|
Pediatric cardiologist with experience in diagnostic catheterization procedures |
1 |
|
Cardiac anesthesiologist |
1 |
|
Specialized scrub nurses |
5 |
|
Cardiac ICU nurses |
6 |
|
Heart-lung machine |
1 |
|
Extracorporeal membrane oxygenator machine |
1 |
|
Intra-aortic balloon pump |
1 |
|
Post-operative cardiac care nurse |
2 |
|
Specialized physiotherapist |
1 |
CONCLUSION
Bhutan’s reliance on neighboring countries for much of the specialized healthcare services including cardiac care is unsustainable in the long run as healthcare cost continues to rise. With the burden of disease shifting from communicable to noncommunicable, CVDs have become the leading cause of all-age mortality, underscoring the urgent need for a localized solution. To tackle this growing challenge, stakeholders must take decisive action.
REFERENCES
1. Yeates K, Lohfeld L, Sleeth J, Morales F, Rajkotia Y, Ogedegbe O. A Global Perspective on Cardiovascular Disease in Vulnerable Populations. Can J Cardiol. 2015; 31(9): 108193. [PubMed] [Full text] [DOI]
2. Li Z, Lin L, Wu H, Yan L, Wang H, Yang H, et al. Global, Regional, and National Death, and Disability-Adjusted Life-Years (DALYs) for Cardiovascular Disease in 2017 and Trends and Risk Analysis From 1990 to 2017 Using the Global Burden of Disease Study and Implications for Prevention. Front Public Health. 2021;9. [PubMed] [Full Text] [DOI]
3. Mensah GA, Roth GA, Fuster V. The Global Burden of Cardiovascular Diseases and Risk Factors: 2020 and Beyond. J Am Coll Cardiol. 2019; 74(20):2529-32. [PubMed] [Full Text] [DOI]
4. Vervoort D, Swain JBD, Pezzella AT, Kpodonu J. Cardiac Surgery in Low- and Middle-Income Countries: A State-ofthe-Art Review. Ann Thorac Surg. 2021;111(4):1394–400. [PubMed] [Full Text] [DOI]
5. Zimmerman MS, Smith AGC, Sable CA, Echko MM, Wilner LB, Olsen HE, et al. Global, regional, and national burden of congenital heart disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc Health. 2020 Mar 1;4(3):185–200. [PubMed] [Full Text] [DOI]
6. Ou Z, Yu D, Liang Y, Wu J, He H, Li Y, et al. Global burden of rheumatic heart disease: trends from 1990 to 2019. Arthritis Res Ther. 2022;24(1). [PubMed] [FullText] [DOI]
7. Antunes MJ. The global burden of rheumatic heart disease: Population-related differences (it is not all the same!). Braz J Cardiovasc Surg. 2020;35(6):958–63. [PubMed] [Full Text] [DOI]
8. Coffey S, Roberts-Thomson R, Brown A, Carapetis J, Chen M, Enriquez-Sarano M, et al. Global epidemiology of valvular heart disease. Nat Rev Cardiol; 2021. Vol. 18, p. 853–64. [PubMed] [FullText] [DOI]
9. Gupta R, Gaur K. Epidemiology of Ischemic Heart Disease and Diabetes in South Asia: An Overview of the Twin Epidemic. Curr Diabetes Rev. 2020;17(9). [PubMed] [DOI]
10. Joshi P, Amin MR, Dorin FA, Dzed L, Lethro P, Swarnkar S, et al. The Dhaka Call to Action to accelerate the control of cardiovascular diseases in South-East Asia. Nat Med. 2024;30(1):19–20. [PubMed] [DOI]
11. Vervoort D, Meuris B, Meyns B, Verbrugghe P. Global cardiac surgery: Access to cardiac surgical care around the world. J Thorac Cardiovasc Surg. 2020 Mar 1;159(3):987-996. [PubMed] [Full Text] [DOI]
12. World Health Organization. Bhutan [Internet]. [cited 2025 Jan 23]. [Full Text]
13. Institute for Health Metrics and Evaluation. Bhutan GBD compare. [Internet] [cited 2025 Jan 24]. [Full Text]
14. Ministry of Health: Annual Health Bulletin 2023. Health Management Information System and Research Section, Policy and Planning Division, Ministry of Health, Royal Government of Bhutan. 165p [Full Text]
15. Bhandari P, Wangmo K. Incidence of congenital heart diseases in children born at Eastern Regional Referral Hospital, Monggar. Bhutan Health J. 2016;2(1):1–4. [Full Text] [DOI]
16. Bhandari P. Catching congenital heart diseases early: the ten- point approach for Bhutan. Bhutan Health J. 2016;2(2):34–6. [Full Text] [DOI]
17. Ministry of Health: Annual Health Bulletin 2024. Health Management Information System and Research Section, Policy and Planning Division, Ministry of Health, Royal Government of Bhutan. 169p. [Full Text]
18. Ministry of Health, Royal Government of Bhutan. 5th National health Survey: Integrated Stepwise Household Survey 2023. Thimphu, Bhutan: inisty of Health; 2024.521p. [Full Text]
19. World Health Observatory. Heart Health Insights in Bhutan [Internet]. [cited 2025 Jan 23]. [Full Text]
20. The Constitution of the Kingdom of Bhutan. 2008; 64p. [Full Text]
21. Khesar Gyalpo University of Medical Sciences of Bhutan. University Profile [Internet]. [cited 2025 Jan 2]. [Full Text]
22. Tenzin K, Dorji T, Dorji G, Lucero-Prisno DE. Health inequities in Bhutan’s free healthcare system: a health policy dialogue summary. Public Health Chall. 2022;1(4). [Full Text] [DOI]
23. National Statistics Bureau. Statistical Yearbook 2023. [Full Text]
24. Penjor T, Wangdi T, Dendup T, Phuntsho S, Pempa, Dorjee K, et al. Policy Brief. Health care financing in Bhutan (2018 - 2020): Evidence from the National Healths Accounts. Ministry of Health. 2021. 3p. [Full Text]
25. Sharma J, Pavlova M, Groot W. Catastrophic health care expenditure and impoverishment in Bhutan. Health Policy Plan. 2023;38(2):228–38. [PubMed] [Full Text] [DOI]
26. Penjor T, Wangdi T, Dendup T, Phuntsho S, Pempa, Dorjee K, et al. Policy Brief. Health care financing in Bhutan (2018 - 2020): Evidence from the National Healths Accounts. Ministry of Health. 2021. 3p. [Full Text] [DOI]
27. The burden of medical referrals. May 31, 2024. Kuensel. [Full Text]
28. Inauguration of first cath lab marks a milestone in cardiovascular care. Sep 07, 2023. Kuensel. [Internet] [Full Text]
29. Revolutionising heart care: Cath Lab’s rapid impact. March 13, 2024. Kuensel. [Internet] [Full Text]
30. Ahmad FB, Anderson RN. The Leading Causes of Death in the US for 2020. JAMA. 2021; 325(18):1829-30. [PubMed] [Full Text] [DOI]
31. Zilla P, Yacoub M, Zühlke L, Beyersdorf F, Sliwa K, Khubulava G, et al. Global Unmet Needs in Cardiac Surgery. Glob heart. 2018; 13(4): 293-303. [PubMed] [Full Text] [DOI]
32. Pandey AR, Dhimal M, Shrestha N, Sharma D, Maskey J, Dhungana RR, et al. Burden of Cardiovascular Diseases in Nepal from 1990 to 2019: The Global Burden of Disease Study, 2019. Glob Health Epidemiol Genom. 2023;2023. [PubMed] [Full Text] [DOI]
33. Al-Ebrahim EK, Madani TA, Al-Ebrahim KE. Future of cardiac surgery, introducing the interventional surgeon. J Card Surg. 2022;37(1):88–92. [PubMed] [Full Text] [DOI]
34. Koirala B. Generating political support for cardiac surgical care in resource-limited contexts: experience from Nepal. AME Surgical Journal. 2022;2:24–24. [Full Text] [DOI]
35. Dindi K, Cain MT, Odera A, Joyce DL, Joyce LD, Leta A, et al. Building cardiac surgical programs in lower-middle income countries. JTCVS Open. 2023; 13:252-9. [PubMed] [Full Text] [DOI]
36. Bhutan launches MBBS programme. Oct 13, 2023. Kuensel. [Full Text]