CASE REPORT
https://doi.org/10.47811/bhj.180
Hypokalemic Periodic Parlaysis Associated with Adrenal Adenoma in a Patient with Conn’s Syndrome: A Case Report
Samuel Noklang1, Pankaj Kumar Kannauje2, Shruthi J3, Imjungba Naklang4, Tepukiel Zaphu5, Nishini Hekha6, Lijanthung S Kithan7, Manong Chohwanglim8
1Department of General Medicine, Zion Hospital and Research Centre, Nagaland, India
2Department of General Medicine, AIIMS, Raipur, India
3Department of Endocrinology, Rajarajeshwari Medical College and Hospital, Bangalore, India
4Department of Surgery, AIIMS, Raebareli
5Department of Urology, Zion hospital and Research Centre, Nagaland, India
6Department of Radiology, Zion Hospital and Research Centre, Nagaland, India
7Department of Pathology and Laboratory Medicine, Zion Hospital and Research Centre, Nagaland, India
8Department of Nephrology, Zion Hospital and Research Centre, Nagaland, India
Corresponding author
Pankaj Kumar Kannauje
drpankajkannauje@aiimsraipur.edu.in
Abstract:
Introduction: Hypokalemic paralysis secondary to Conn’s syndrome is rare. The most common presentation of this condition is hypertension, which may be asymptomatic or range from mild to severe to refractory. Case Report: A 34-year-old hypertensive female presented with acute onset of lower limb weakness. She reported two similar episodes in the past. She had profound hypokalemia and further evaluation revealed high aldosterone and low renin levels, suggesting an adrenal adenoma. She was managed with antihypertensives and spironolactone. After CT confirmation of a right adrenal adenoma, she underwent surgery. She showed significant improvement in both her symptoms and laboratory parameters after surgery, and is doing well on her follow-up. Conclusion: This case illustrates that a high index of suspicion leads to early recognition and timely management of an unusual and potentially severe clinical manifestation of primary hyperaldosteronism in the form of hypokalemic periodic paralysis, especially in the setting of unexplained hypertension.
Keywords: Adrenal Adenoma; Aldosteronism; Hypokalemia; Hypertension; Periodic Paralysis
INTRODUCTION
Primary hyperaldosteronism (PA), also known as Conn’s syndrome, is caused by aldosterone hypersecretion from the adrenal glands1. It is seen in 5-10% of hypertensive patients and increases to 25-30% in those with resistant hypertension. The various subtypes of PA include bilateral adrenal hyperplasia (60-70%), aldosterone-producing adenoma (30-40%), and rare subtypes (<1%) like glucocorticoid remediable aldosteronism and ectopic aldosterone-producing tumours1. The classical presentation includes hypertension, hypokalemia and metabolic alkalosis. However, patients can also present with manifestations of hypokalemia such as muscle weakness, and symptoms of alkalosis such as excessive urination, polydipsia, tetany, paraesthesia, and cramps1.
Aldosterone acts on distal tubules and collecting ducts of the kidney, resulting in sodium and water reabsorption and potassium excretion, corresponding to the symptoms of hypertension and hypokalemia. It also stimulates hydrogen ion secretion in the distal nephron resulting in metabolic alkalosis, which in turn impairs the repolarization of skeletal muscles and disrupts neuromuscular transmission, causing periodic paralysis and cramps with tetany2.
Although hypokalemia occurs in 9-37% of patients with PA, hypokalemic myopathy due to PA is rarely reported2. It is usually seen when the plasma potassium concentration falls below 2.5 mEq/L but can occur at higher levels if the onset is acute3. There is a need to differentiate between hereditary hypokalemic periodic paralysis and those secondary to conditions like thyrotoxic periodic paralysis, from that of Conn’s syndrome. This differentiation is crucial for guiding disease management and determining the patient’s prognosis4.
Herein, we describe the case of a young hypertensive female patient who presented to the hospital with hypokalemic periodic paralysis due to a primary adrenal adenoma, along with its management and follow-up.
CASE REPORT
A 34-year-old Naga lady presented to the emergency department on April 2023 with complaints of gradual onset weakness in her lower extremities for 3 days and difficulty in walking for 1 day. The patient had a history of hypertension since 2012 but had been taking amlodipine 10mg once daily irregularly. She had experienced similar episodes of limb weakness in 2019 and 2022, which had resolved after a few days of hospitalization and treatment. However, her symptoms were not fully investigated. Her family history was non-contributory.
On physical examination, her body mass index (BMI) was 25.8 kg/m2, pulse rate was 82 beats per minute, and blood pressure was 170/100 mmHg on the right arm and 166/96 mmHg on the left arm. She did not exhibit any peripheral manifestations of hypo or hyperthyroidism, acromegaly or Cushing’s syndrome. Cardiovascular, respiratory and abdominal examinations were unremarkable. Medical Research Council (MRC) grading of muscle power was 5 in both upper limbs, while it was 2 and 3 in the proximal and distal groups of lower limbs, respectively. Knee and ankle reflexes were diminished, and the plantar response was mute. Sensory examination was normal.
Laboratory investigations revealed normal complete blood count, blood glucose, blood urea nitrogen, creatinine, liver function and urinalysis. However, she had hypokalemia with a serum potassium of 2.9 mmol/L. Her previous medical records also revealed a serum potassium as low as 2.3 mmol/L. Her electrocardiogram showed normal sinus rhythm, biphasic T waves, and prominent U waves with left ventricular hypertrophy changes (Figure 1). Chest X-ray, abdominal ultrasound, and renal artery doppler were unremarkable. She was treated with intravenous potassium chloride (60 mEq/day) and oral potassium chloride (80 mEq/day). Clonidine and amlodipine were used as antihypertensive agents, and later spironolactone was added, following which her paraparesis substantially improved after 2 days.
Meanwhile, further evaluation continued. Her autoantibody profile, including antinuclear antibody (ANA), anti-double stranded DNA (anti-dsDNA), and anti-extractable nuclear antigen antibodies (anti-ENA antibodies), was non- contributory. A suspicion of primary hyperaldosteronism as the cause of hypertension with hypokalemic periodic paralysis was raised. This was confirmed by a raised plasma aldosterone level and suppressed plasma renin activity. Table 1 summarises the significant laboratory findings. Contrast-enhanced computed tomography (CECT) of the upper abdomen revealed a small, oval soft tissue mass measuring 1.1 x 1.1 x 0.8 cm between the limbs of the right adrenal gland, consistent with an adrenal adenoma (Figure 2). The left adrenal gland appeared normal.
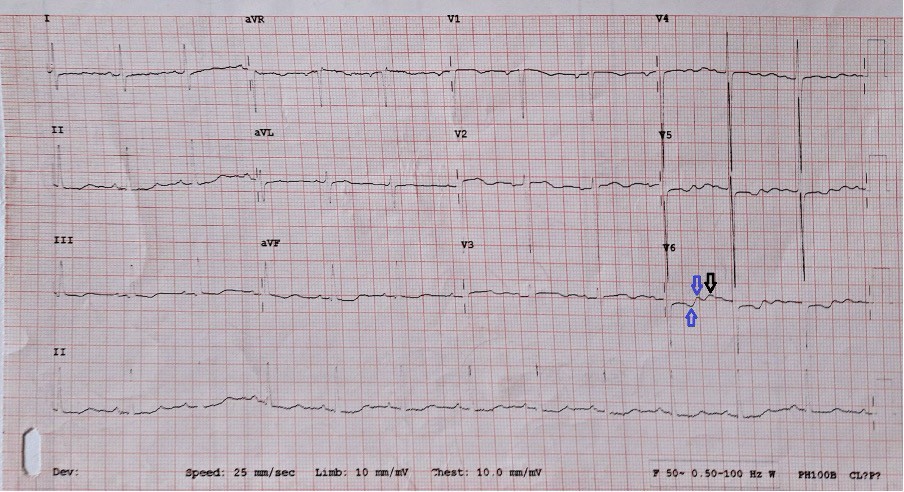
Figure 1: A 12-lead ECG on admission. Blue arrows indicate the biphasic T waves and black arrow indicates the prominent U waves.
Table 1: Baseline laboratory investigations of the patient.
|
Parameter |
Observed Value |
Reference Range |
|
Serum Potassium |
2.3 mmol/L |
3.5 – 5.1 mmol/L |
|
Serum Sodium |
143 mmol/L |
136 – 145 mmol/L |
|
Serum Chloride |
99 mmol/L |
97 – 111 mmol/L |
|
Serum Magnesium |
0.67 mmol/L |
0.65 – 1.05 mmol/L |
|
Serum Calcium |
8.3 mg/dL |
8.1 – 10.4 mg/dL |
|
Plasma aldosterone level |
44.6 ng/dl |
3.0 to 16 ng/dL in lying down position |
|
Plasma Renin Activity |
< 0.10 ng/mL/h |
0.15 to 2.33 ng/mL/h in lying down position |
|
Fasting 8 am Serum Cortisol |
17 mcg/dL |
5 to 23 mcg/Dl |
|
Overnight Dexamethasone Suppression Test |
1.17 mcg/dL (Appropriately suppressed) |
< 1.8 mcg/dL |
|
Plasma Free Metanephrine |
5.40 pg/mL |
< 90.0 pg/mL |
|
Plasma Nor-Metanephrine |
55.67 pg/mL |
< 190.0 pg/mL |
|
TSH |
1.74 µIU/mL |
0.27 – 4.20 µIU/mL |
|
Thyroxine (T4) |
63.82 nmol/L |
66.00 – 181.0 nmol/L |
|
Triiodothyronine (T3) |
0.88 nmol/L |
1.30 – 3.10 nmol/L |
|
ESR |
44 mm 1st Hr |
Female: 0 – 20 mm 1st Hr |
|
Urinalysis |
pH: 7.5 Protein: 2+ RBCs: Nil Casts: Nil |
pH: 4.5 – 8 Protein: Negative to trace RBCs: 0 – 2/hpf Casts: 0 – 5 |
TSH- Thyroid Stimulating Hormone, RBC- Red Blood Cells, hpf- high power field
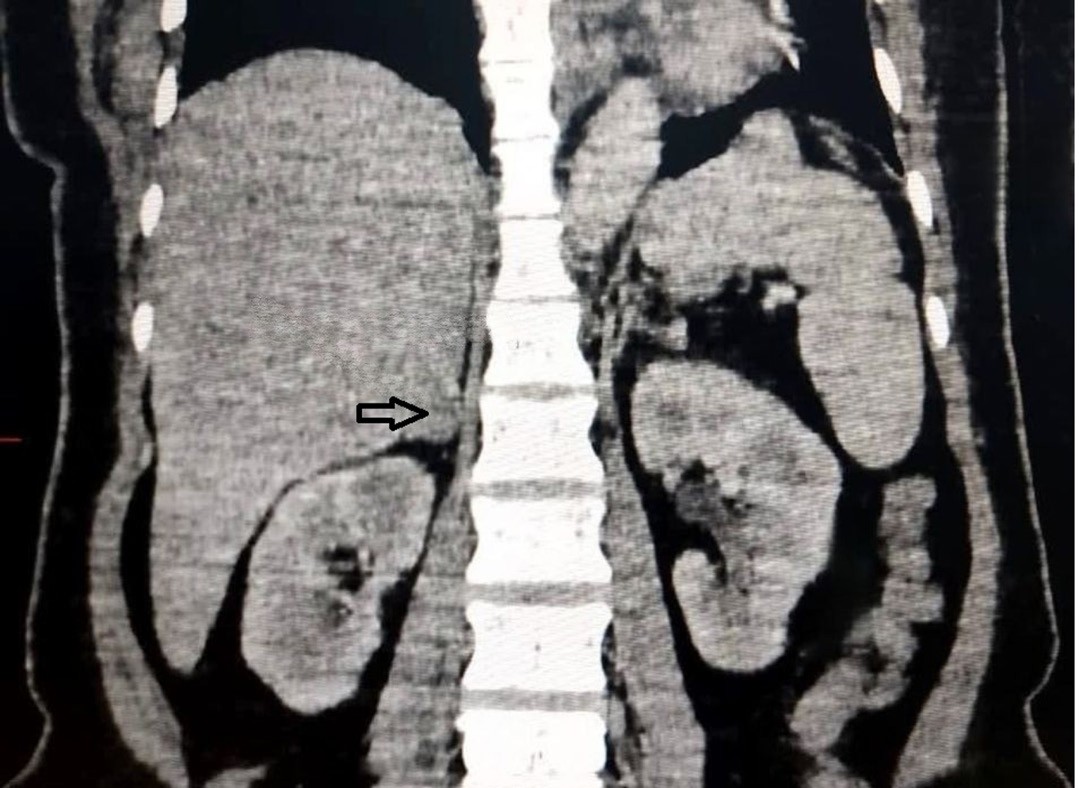
Figure 2: CECT abdomen of the patient showing a right- sided adrenal adenoma (black arrow).
After this thorough evaluation, she was scheduled to undergo surgical removal of the adenoma via right open adrenalectomy. The surgery was uneventful, and the adenoma was successfully removed (Figure 3a and 3b). Histopathology showed features suggestive of an adrenocortical adenoma (Figure 4).
Post-surgery, her potassium level improved to
3.8 mmol/L within 48 hours. Her symptoms and blood pressure returned to normal without the need for any antihypertensives. She continued to have her serum potassium levels monitored every 12 hourly initially, and later on a daily basis. It remained within the normal range without any potassium supplementation. At her 2-month follow up, she reported no recurrence of symptoms, hypertension or hypokalemia.
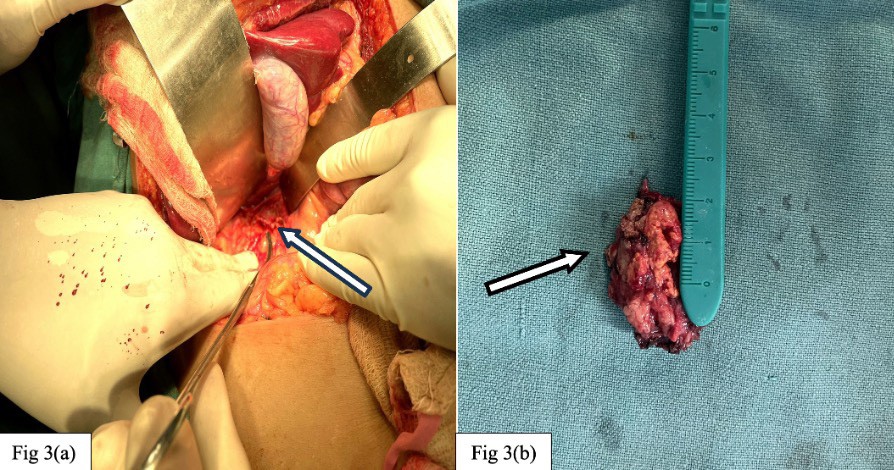
Figure 2: CECT abdomen of the patient showing a right- sided adrenal adenoma (black arrow).
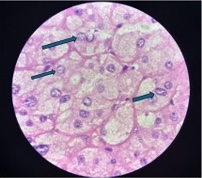
Figure 4: H&E stained slide of the resected adrenal adenoma, depicting a well-circumscribed tumour in large nests with nuclear pleomorphism, bland nuclei (arrows) and abundant clear cytoplasm with well-defined cell borders
DISCUSSION
PA (Conn's syndrome) is the most common form of endocrine hypertension characterized by adrenal overproduction of aldosterone5-7. The common causes of PA are bilateral adrenal hyperplasia (60-70%) and aldosterone-producing adenoma (30-40%)1. Excess aldosterone is known to cause hypertension in most cases, but it is not often associated with hypokalemia and only rarely leads to hypokalemic paralysis8. Kotsaftis et al. identified unilateral adrenal hyperplasia as the underlying cause of primary hyperaldosteronism which manifested as hypokalemia- induced myopathy9. In addition, Kayal et al. found only 1 patient (1.78%) in a study population of 56 adults as having primary hyperaldosteronism-induced hypokalemic paralysis10.
Hypokalemic periodic paralysis (HypoPP) is a rare neuromuscular disorder with an estimated prevalence of 1 in 100,000 population11. It is the most common form of periodic paralysis, affecting males more than females4. Although most cases are hereditary, secondary causes of periodic paralysis (PP), like thyrotoxic hypokalemic PP, have been reported in the literature. It is hence essential to differentiate between Conn’s syndrome and HypoPP to aid in the diagnosis and management. Making the correct diagnosis is important since secondary HypoPP can be treated with antithyroid drugs, hereditary cases with spironolactone, while Conn’s syndrome requires surgery as the definitive treatment of choice.
Basic biochemical tests in Conn’s syndrome may show mild metabolic alkalosis, hypernatremia (usually < 150 mEq/L), and hypokalemia which is seen in 60% of the cases and absent in 40%10. The aldosterone-to-renin ratio (ARR), where a low renin level is seen, is the single most important feature that raises suspicion of primary aldosteronism. Low renin levels may be present alone or together with an inappropriately high and non- suppressible plasma aldosterone level10.
A high-resolution computed tomography of the abdomen needs to be performed in all patients after the initial biochemical confirmation. It will help ascertain if the cause is a unilateral or bilateral aldosterone-producing adenomas (APA). APAs are known to be small in size (< 2 cm) and hypodense in nature (HU < 10), whereas patients with idiopathic adrenal hyperplasia (IAH) may have normal or bilateral adrenal masses on CT12. Adrenal venous sampling is considered for patients with a high probability of APA but with normal CT findings or bilateral adrenal masses on CT12.
The treatment of choice for APA with unilateral adrenal hyperplasia is always surgical, preferably a unilateral laparoscopic adrenalectomy, which results in complete resolution of hypertension in 35 - 70% of patients and normalisation of potassium levels12. Despite the known advantages of minimal access surgery, such as reduced risk of infection and postoperative pain, our patient underwent an open adrenalectomy due to the rarity of the case and the limitations of the small health centre. Patients who refuse surgery or have contraindications to surgery, such as advanced age and multiple comorbidities, and those with bilateral adrenal hyperplasia and invasive adrenal malignancy, are supplemented with mineralocorticoid receptor antagonists like spironolactone with great effectiveness12. Patients who are not on any medications are found to have severe target organ damage like left ventricular hypertrophy, albuminuria, hypertensive retinopathy, and cognitive dysfunction with stroke12.
As per the Primary Aldosteronism Surgery Outcome (PASO) guidelines, outcomes are defined as complete, partial, or absent, based on blood pressure control, use of antihypertensive medications, plasma potassium levels, aldosterone concentrations, and renin concentrations or activities. The first post-surgical assessment, including serum potassium and blood pressure, should be done within three months of the surgery. Subsequent assessments should be conducted 6-12 months later to evaluate outcomes and then annually, to assess for any disease persistence or recurrence13.
The sole independent predictor of complete biochemical success is higher preoperative blood pressure. Complete clinical success is independently associated with female sex, younger age, lower use of antihypertensive medications (defined in terms of daily dose), and the absence of left ventricular hypertrophy13. The presence of these factors has contributed to the positive outcome in our patient.
CONCLUSION
A very high index of suspicion is required in patients with hypertension, hypokalemia, metabolic alkalosis, and periodic paralysis to diagnose primary aldosteronism and prevent organ damage. This case report highlights the need for multidisciplinary collaboration among physicians, endocrinologists, nephrologists, neurologists, and surgeons to optimize patient care via early recognition, prompt diagnosis, and tailored management strategies.
ACKNOWLEDGEMENT
We would like to thank the consultants, medical officers and staff of the Department of General Medicine, Zion Hospital, Dimapur for their contributions and special efforts in this case.
REFERENCES
1. Laurel MT, Kabadi UM. Primary hyperaldosteronism. Endocr Pract. 1997;3(1):47-53. doi: 10.4158/EP.3.1.47.
2. Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93(9):3266-81. [PubMed] [Full Text] [DOI]
3. Kogika MM, de Morais HA. A Quick Reference on Hypokalemia. Vet Clin North Am Small Anim Pract. 2017;47(2):229-34. [PubMed] [DOI]
4. Nicoletti T, Modoni A, Silvestri G. Secondary hypokalemic periodic paralysis as a rare clinical presentation of Conn syndrome. Clin Neurophysiol. 2018;129(11):2505-6. [PubMed] [DOI]
5. Mulatero P, Monticone S, Bertello C, Tizzani D, Iannaccone A, Crudo V, et al. Evaluation of primary aldosteronism. Curr Opin Endocrinol Diabetes Obes. 2010;17(3):188-93 [PubMed] [DOI]
6. Onder A, Kendirci HNP, Bas VN, Agladioglu SY, Cetinkaya S, Aycan Z. A pediatric Conn syndrome case. J Pediatr Endocrinol Metab. 2012;25(1-2):203-6 [PubMed] [DOI]
7. Ganguly A. Primary aldosteronism. N Engl J Med. 1998;339(25):1828-34. [PubMed] [Full Text] [DOI]
8. Rajesh R, Bhagat T, Tek CY, Vijay PY. Hypokalemic Periodic Paralysis: A Rare Presenting Manifestation of Conn’s Syndrome. J Endocrinol Metab and Elmer Press Inc. 2015;5(1-2):196-8. [Full Text] [DOI]
9. Kotsaftis P, Savopoulos C, Agapakis D, Ntaios G, Tzioufa V, Papadopoulos V, et al. Hypokalemia induced myopathy as first manifestation of primary hyperaldosteronism – an elderly patient with unilateral adrenal hyperplasia: a case report. Cases J. 2009;2:6813. [PubMed] [Full Text] [DOI]
10. Kayal AK, Goswami M, Das M, Jain R. Clinical and biochemical spectrum of hypokalemic paralysis in North: East India. Ann Indian Acad Neurol. 2013;16(2):211-7. [PubMed] [Full Text] [DOI]
11. Fontaine B. Periodic paralysis. Adv Genet. 2008;63:3-23. [PubMed] [Full Text] [DOI]
12. Hamrahian AH, Loachimescu AG, Remer EM, Motta- Ramirez G, Bogabathina H, Levin HS, et al. Clinical utility of noncontrast computed tomography attenuation value (hounsfield units) to differentiate adrenal adenomas/ hyperplasias from nonadenomas: Cleveland Clinic experience. J Clin Endocrinol Metab. 2005;90(2):871-7. [PubMed] [DOI]
13. Williams TA, Lenders JWM, Mulatero P, Burrello J, Rottenkolber M, Adolf C, et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: an international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 2017; 5(9):689–699. [PubMed] [Full Text] [DOI]

|
|
|
|
|
|
|
|
