CASE REPORT
https://doi.org/10.47811/bhj.179
Bilateral retinoblastoma presenting as leukocoria in unilateral eye: a case report
Phuntsho Dorji1,2, Samten Dorji1,2, Dechen Wangmo1,2, Tshering Dorji1
1Gyalyum Kesang Choeden Wangchuck National Eye Centre, Jigme Dorji Wangchuck National Referral Hospital, Thimphu, Bhutan
2Faculty of Post Graduate Medicine, Khesar Gyalpo University of Medical Sciences of Bhutan, Thimphu, Bhutan
Corresponding author
Phuntsho Dorji
pdorji@jdwnrh.gov.bt
Abstract:
Retinoblastoma (RB) is the most common ocular tumour in childhood. Presentations include leukocoria, strabismus, decreased vision and painful blind eye. RB can have extraocular extension into the orbit and also metastasise distantly to the brain. We present the case of a 2-year-old child with RB in both eyes, advanced stage in left eye and early stage in the right eye. The left eye was treated with chemoreduction followed by enucleation. The histopathology examination of enucleated eye showed RB cells with no invasion of the optic nerve. The right eye was salvaged after treatment with cryotherapy and laser therapy. This case is significant as RB is a rare disease that was not previously reported from Bhutan. If a child presents with leukocoria, paediatricians and ophthalmologists should have a high suspicion of RB. Timely referral to an ocular oncologist and vitreoretinal specialist is crucial to save vision and the child’s life.
Keywords: Cryotherapy; Enucleation; Leukocoria; Retinoblastoma; Strabismus.
INTRODUCTION
Retinoblastoma (RB), a malignant tumour of the eye caused by mutation in the Rb1 gene, is one of the most common tumours in children1. It commonly presents as whitish reflex (leukocoria) and squinting of the eye2. It originates from the retina and it can have either an endophytic or exophytic growth pattern. If left untreated, RB has a high risk of ocular morbidity with a potential for exudative retinal detachment, glaucoma, strabismus and loss of vision2. There may also be extraocular extension of the tumour into the orbit and brain. Furthermore, it is also associated with a high risk of mortality2. Here, we report a case of RB which presented with advanced disease in the left eye and early stage in the right eye.
CASE REPORT
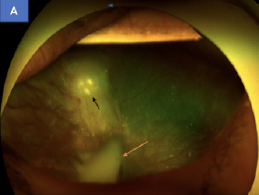
A 2-year-old boy presented to the National Eye Center with a complaint of whitish reflex in the left eye, noticed by the parents for two weeks. There was no history of trauma, eye pain, redness, deviation of eyes or any significant past ocular history. The child was born at term. On examination, the patient was noted to be fixing and following light in the right eye, whereas the left eye had no perception of light. On distant direct ophthalmoscopy, there was a whitish fundal glow (leukocoria) in the left eye and normal fundal glow in right eye (Figure 1A and 1B). The anterior segment examination of both eyes were normal. The posterior pole of the right eye was normal with a clear media, pink optic disc and a cup disc ratio of 0.3:1. The left eye had a whitish mass inside the posterior segment. The peripheral retina of both eyes could not be examined as the child was uncooperative at the eye clinic.
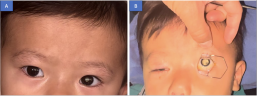
Figure 1A: White reflex (leukocoria) in the left eye. 1B: Dilated pupil showing prominent leukocoria in left eye.
An examination under anaesthesia was performed for a detailed fundus examination which revealed three whitish lesions at the level of equator in the superior and superonasal retina of the right eye. The lesion sizes were about one third size of optic disc. In the left eye, there was a whitish fluffy mass involving almost two third of vitreous cavity with exudative retinal detachment. There was vitreous as well as subretinal seeding of the whitish lesion (Figure 2). The examination findings were suggestive of bilateral RB. An ultrasound B-scan was done in both eyes. There was moderate to high reflectivity in A-scan images and heterogenous vitreous echoes along with exudative retinal detachment in the B-scan of left eye (Figure 3). The right eye ultrasound B scan was normal. The computed tomography scan of the orbit showed a partially calcified posterior intraocular mass of 1x 0.6 x 1.2 cm with retinal detachment in the left eye (Figure 4). The brain and optic nerve of both eyes were normal. A working diagnosis of bilateral RB, stage A in the right eye and stage E in the left eye was reached.
Figure 2: Fundus image of left eye showing retinoblastoma tumour in vitreous cavity (orange arrow) and behind retina (black arrow).
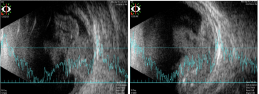
Figure 3: Ultrasound B scan showing endophytic growth of retinoblastoma tumour in left eye.
The child was referred to India for ocular oncology intervention. Cerebrospinal fluid and iliac crest bone marrow aspirate was sent for cytopathology examination. Both reports were negative for RB cells. Magnetic resonance imaging of brain and orbit revealed a dome shaped lesion posterior to equator with associated retinal detachment in left eye. There were tiny elevated lesions at the posterior and superior retina of the right eye. There was no extraocular extension to the orbit and brain. The patient underwent three cycles of chemotherapy, comprising a combination of vincristine, etoposide and cisplatin. Left eye enucleation was performed after the first cycle of chemotherapy. The enucleated eye was sent for histopathology examination, which confirmed RB with no involvement of optic nerve (Figure 5A and 5B).The right eye was treated with cryotherapy and transpupillary thermotherapy (TTT).
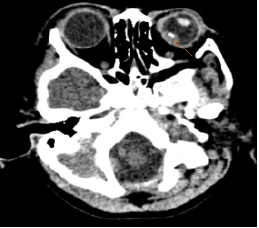
Figure 4: CT scan showing a well-defined lesion with calcification (orange arrow) in the left orbit.
The patient was followed up for eight months after the treatment. Currently, the patient has a prosthetic eye in the left orbit with no recurrence of tumour in the orbital socket. There was no evidence of new lesions in the right eye at the last follow up exam 8-months after treatment.
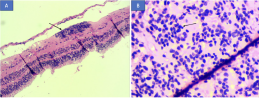
Figure 5A: Histopathology of enucleated left eye showing viable tumour cells (black arrow) Figure 5B: Extensive differentiation of tumour cells known as fleurettes (black arrow).
DISCUSSION
RB is a malignant tumour of the eye, typically occurring in children under five years1. RB can be hereditary or sporadic. Most children with RB present with leukocoria (56%), strabismus (20%), red painful eye (7%) and poor vision (5%)2. Parents bring affected children to an eye centre when they notice a whitish lesion in the eye or when the child develops squinting of the eye. The International Classification of Retinoblastoma (ICRB) classifies RB into five groups depending on the size of tumour, location, tumour seeding, optic nerve involvement and orbital extension3. The groups are named as Group A, B, C, D and E. In our case, the patient was grouped as group A in right eye (owing to size less than or equal to 3mm) and Group E (extensive RB) in the left eye.
There are different treatment options depending on the categories of RB ranging from laser photocoagulation, transpupillary thermotherapy (TTT), cryotherapy, systemic chemotherapy, intravitreal chemotherapy to enucleation2,3. Cryotherapy and TTT are indicated for small tumours (less than 3.5 mm in size) without vitreous and sub retinal seeding4,5. In our patient, the right eye was treated with transconjunctival cryotherapy and TTT since the lesions were less than 3.5 mm in size. For group E RB, chemoreduction followed by enucleation is the preferred treatment6. Accordingly, our patient received three cycles of chemoreduction following which the left eye was enucleated and prosthetic eye implant was done.
Mortality of patients with RB depends on the extent of optic nerve involvement. The mortality is as high as 42% if the optic nerve is involved posterior to lamina cribrosa7. Our patient had no involvement of the optic nerve, which is a good prognostic indicator. A close follow up is needed to monitor disease recurrence inside the eye as well as in the orbit. In our patient, there was no recurrence of RB at eight months of follow up. The patient is scheduled for ongoing follow up.
RB needs to be detected early for treatment to be initiated on time, in order to ensure that the child doesn’t lose his vision nor his life. This mandates clinicians to have a high degree of suspicion of RB in children presenting with leukocoria and instituting timely referral to the ophthalmologist.
ACKNOWLEDGEMENT
We would like to thank the patient’s parents for allowing us to use de-identified clinical details and images for publication purpose. We are indebted to the staff of the diagnostic unit at the National Eye Centre and Sankara Nethralaya, Chennai for providing us the images and histopathology pictures.
REFERENCES
1. Ortiz MV, Dunkel IJ. Retinoblastoma. J Child Neurol.2016;1(2):227–36. [Pubmed] [Full Text] [DOI]
2. Gupta AK, Meena J P. A narrative review of retinoblastoma and recent advances in its management. Pediatr Med. 2020;3:20.[Full Text] [DOI]
3. Shields CL, Mashayekhi A, K. Au Angela, C Craig, LAnn, Meadows AT, et al. The International Classificationof Retinoblastoma Predicts Chemoreduction Success. Ophthalmology. 2006;113:2276 –80.[Pubmed] [Full Text] [DOI]
4. Rao R, Hanovar SG. Retinoblastoma. Indian J Pediatr. 2017;84:937-44.[Pubmed] [Full Text] [DOI]
5. Shields CL, Santos MC, Diniz W, Gunduz K, Mercado G,Cater JR et al. Thermotherapy for retinoblastoma. ArchOphthalmology. 1999; 117:885-93. [Pubmed] [Full Text] [DOI]
6. Zhao J, Dimaras H, Massey C, Xu X, Huang D, Li B et al. Pre-enucleation chemotherapy for eyes severely affected by retinoblastoma masks risk of tumor extension and increases death from metastasis. J Clin Oncol. 2011; 29:845-51[Pubmed] [Full Text] [DOI]
7. Shields CL, Shields JA, Baez K, Cater RI, Potter PD. Optic nerve invasion of retinoblastoma: metastatic potential and clinical risk factors. Cancer. 1994; 73:692-8. [Pubmed] [Full Text] [DOI]


|
|
|
|
|
|
|
|