CASE REPORT
https://doi.org/10.47811/bhj.182
Bilateral undescended testes with intra-abdominal left testicular seminoma: a case report
Kinley Sangay Dorji1, Tandi Wangdi2
1Department of Radio-diagnosis & Imaging, Jigme Dorji Wangchuck National Referral Hospital, Thimphu, Bhutan
2Trashigang Hospital, Trashigang, Bhutan.
Corresponding author:
Kinley Sangay Dorji
ABSTRACT
Undescended testis is a common congenital male genitalia anomaly characterized by absence of one or both testes in the scrotum. It is seen in approximately 3% of full-term male newborns and 30% of preterm male neonates. The most feared complication of undescended tests is testicular cancer. We present a case of a 31-year-old male with lower abdominal pain, fullness and urinary urge incontinence for 2 weeks’ duration. On physical examination, there was a firm non-tender suprapubic mass and absence of testes in the scrotum. A contrast enhanced computed tomography scan showed a well circumscribed lobulated heterogeneous mass in the pelvic cavity drained by the left testicular vein which was later confirmed to be a left testicular seminoma by histopathology report.
INTRODUCTION
Undescended testis is the most common congenital anomaly involving the male genitalia which is characterized by the absence of one or both testes in the scrotum by four months of age (or corrected age for premature infants)1. It occurs in approximately 3% of the full-term male newborns, decreasing to about 1% by 6 months to 1 year of age2,3. The incidence is much higher in preterm male neonates, reaching up to 30%2. The most feared complication is the development of testicular cancer, which is 4-7.5 times higher as compared to normally located testis4. We hereby report a case of a middle-aged adult male who presented with a large pelvic mass in the background of bilateral undescended testes.
CASE REPORT
A 31-year-old male presented to the surgical outpatient department at Trashigang Hospital with lower abdominal pain and fullness associated with urinary urge incontinence for 2 weeks. There was no fever, loss of appetite or loss of weight. He has remained childless despite 10 years of marriage and cohabitation with his spouse, suggesting possible subfertility. Physical examination demonstrated a mass at the suprapubic region which was firm and non-tender. The lower end of the mass could not be palpated. The genitalia examination revealed absence of testes in the scrotum. Upon further inquiry, the patient reported that he was born via home delivery. He also reported experiencing scrotal pain and swelling during adolescence but never sought medical advice. He reported not noticing the absence of testes until the genital examination conducted during the current visit.
An ultrasound scan confirmed the presence of the pelvic mass which was seen as a well-defined hypoechoic mass, measuring about 10.0 x 8.8 cm, in the hypogastric region. However, the origin of the mass could not be ascertained by the scan. The patient was therefore referred to the Eastern Regional Referral Hospital at Mongar for further diagnostic evaluation including tumour markers and computed tomography (CT) scan.
Tumour markers were elevated with alpha fetoprotein (AFP) at 182.00 IU/ml, beta-human chorionic gonadotrophin (beta-hCG) at 90.00 mIU/ml and lactate dehydrogenase (LDH) at 7010.97 U/L. The contrast enhanced computed tomography (CECT) scan of the abdomen and pelvis showed a large well circumscribed lobulated heterogeneously enhancing mass, measuring about 19.1 x 13.5 x 17.1 cm, in the pelvic cavity extending up to the lower abdomen [Figure 1]. The mass was noted to be drained by the left pampaniform plexus and testicular vein. The left testis could not be identified separately, indicating that the intra-abdominal mass was the left testis [Figure 2]. Another well circumscribed lobulated mass, measuring about 6.2 x 4.8 x 6.3 cm, was seen at the left para-aortic region which was consistent with malignant lymphadenopathy. In addition, a small round enhancing soft tissue density lesion, measuring about 3.5 x 2.6 cm, was seen at the right inguinal canal with surrounding collection suggestive of an undescended right testis with hydrocele.
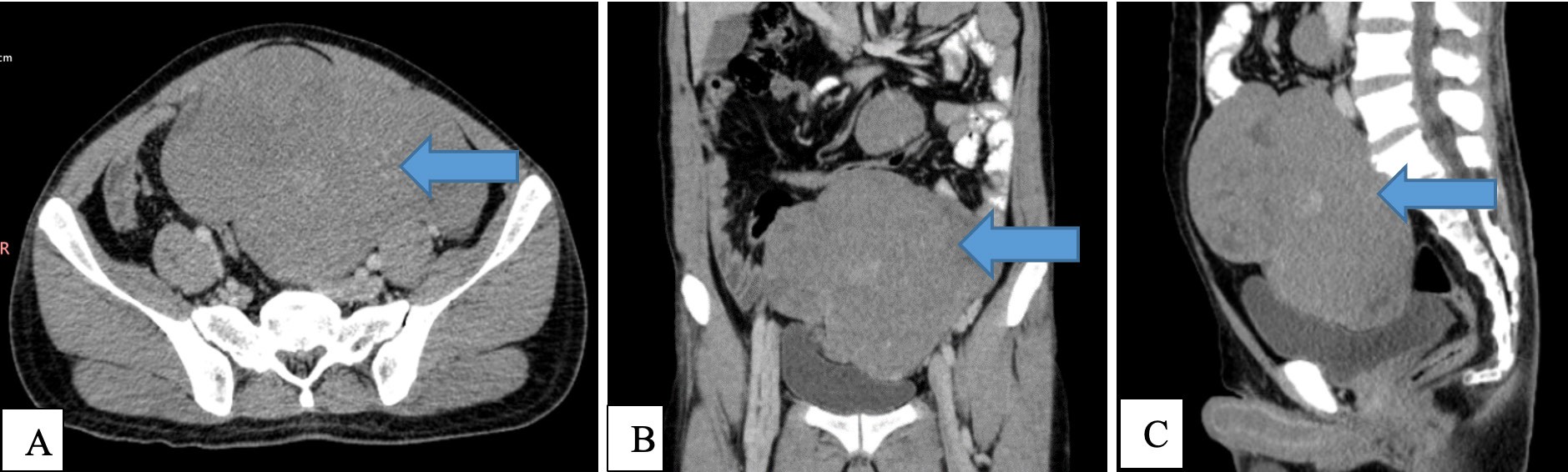
Figure 1. CECT scan showing a large well circumscribed lobulated heterogeneously enhancing mass (blue arrow) in the pelvic cavity extending up to the lower abdomen with local mass effect in Axial (A), Coronal(B) and Sagittal(C) views.
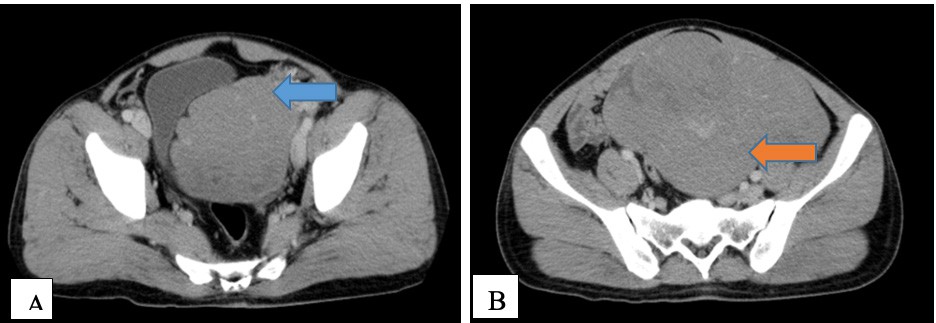
Figure 2. CECT images in the axial view images in the axial view showing A) Left pampaniform plexus (blue arrow) and
B) Left testicular vein (orange arrow) draining the abdomino- pelvic mass.
The patient underwent laparotomy with excision of the abdominopelvic mass and left retroperitoneal para-aortic mass along with right transabdominal high inguinal orchiectomy. Intra-operatively, the left intra-abdominopelvic mass was noted to be about 20 x 20 cm in size and 18 kg in weight, while the left infra-renal para-aortic mass measured about 7 x 7 cm [Figure 3A and 3B]. The right testis was noted to be atrophic [Figure 3C]. Minimal ascites was also noted in the pelvis.
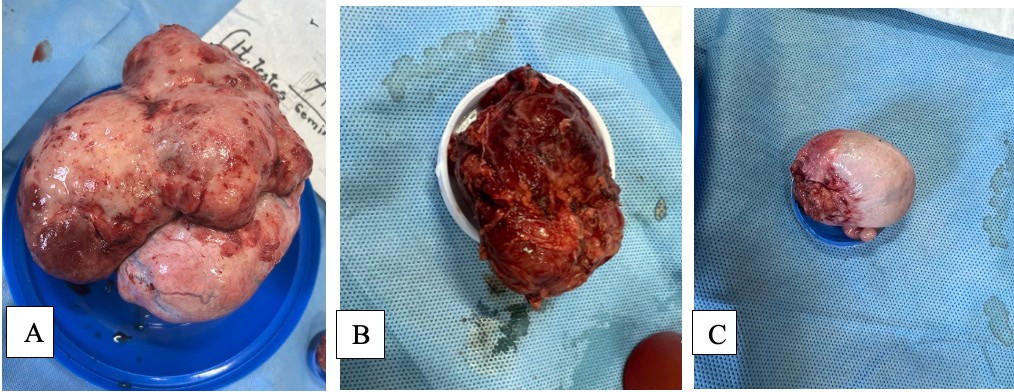 |
Figure 3. Gross post-operative specimens of A) Left testis seminoma, B) Left para-aortic mass and C) Right testis.
The post-operative period was uneventful and he was discharged after 5 days. The histopathological examination confirmed that the abdominopelvic mass was a seminoma while the left para-aortic mass showed morphological features consistent with metastatic seminoma. The right testicular mass was benign. The ascitic fluid which was sent for cytology was suspicious for malignancy-category IV.
The patient was then referred to the Jigme Dorji Wangchuck National Referral Hospital (JDWNRH) at Thimphu for oncology consultation and further management. He ultimately got referred to India where he received chemotherapy with 3 cycles of bleomycin, etoposide and platinum (BEP) with each cycle lasting 3 weeks. No radiotherapy was given.
As of now, the patient is doing well clinically. The latest CT done in JDWNRH showed no evidence of recurrence or residual tumour, lymphadenopathy or metastases. Levels of AFP, beta-hCG and LDH were all within normal limits. He is being followed up on a 3 monthly basis with tumour markers.
DISCUSSION
The testis develops from the genital ridge originating from the intermediate mesoderm inside the abdomen which then descends into the scrotum by 30-33 weeks of gestation. During this process, the migration of the testis can be arrested, resulting in an undescended testis anywhere along its developmental path, from the lower pole of the kidney to the external inguinal ring. Nearly 66% of the undescended testis are located at the external inguinal ring, 16% within the inguinal canal, and 10% inside the abdomen4. It can be unilateral or bilateral, with bilateral cryptorchidism occurring in about 10% of the cases5. Our patient presented with bilateral undescended testis wherein the right testis was located in inguinal canal while the left testis was inside the abdomen.
While untreated cryptorchidism can result in several complications such as infertility, testicular torsion, inguinal hernias and physiological impacts, the most feared complication is the development of testicular cancer which ranges from 3.5- 14.5%6,7. This risk increases up to 200 times when the undescended testis is located intra abdominally8. Malignant transformation of an undescended testis has a peak incidence in the third and fourth decades of life, aligning with our patient’s age9. The most common type of testicular cancer is seminoma (43%) followed by embryonic carcinoma (28%), teratocarcinoma (27%) and choriocarcinoma (2%)8. In our patient, the intra-abdominal left testicular mass was diagnosed as seminoma.
Intra-abdominal testicular cancers are often asymptomatic and are typically diagnosed incidentally during evaluation for other pathologies. Occasionally, they may present with symptoms such as abdominal pain, distension or compressive symptoms of the gastrointestinal and genitourinary tracts. In our patient, urinary urge incontinence was a notable symptom.
The imaging findings of intra-abdominal testicular cancer, whether by ultrasound, CT or magnetic resonance imaging (MRI), are non-specific. The lesion is usually seen as a well- defined pelvic or retroperitoneal mass. This poses a diagnostic challenge for the radiologists as it can often be mistaken for mesenteric or retroperitoneal sarcoma or lymphadenopathy. However, the presence of the “testicular vascular pedicle” sign, characterised by testicular vessels entering and exiting the mass, is highly specific for an intra-abdominal testicular mass10. When combined with the absence of testis in the scrotum, this finding aids in the diagnosis. In our case, the pelvic mass was observed to be drained by a dilated left testicular pampaniform plexus, which drained into the left testicular vein and subsequently into the left renal vein, consistent with testicular vascular pedicle sign. In addition, a left para-aortic mass was observed indicating nodal metastases which was consistent with malignant nature of the mass. This was confirmed by the histopathology report.
Genitalia examination is an important component of the neonatal evaluation which must be performed on all newborns. In male neonates born at full term, scrotum should be palpated for testes. The early detection of undescended testes followed by early placement in the scrotal position is shown to prevent complications such as infertility, testicular malignancy, facilitate future examination of testes, correct inguinal hernia which frequently accompanies undescended testes and minimize risk of torsion. Unfortunately, our patient had a history of home delivery and most likely did not have proper neonatal evaluation which is mandatory in institutional deliveries. In addition, he did not seek medical consultation when he experienced recurrent scrotal pain and swelling during his adolescence, thereby leading to complications such as infertility and testicular germ cell tumour. Apart from the medical complications, there are considerable psychological, emotional, and financial strains. He underwent divorce from his spouse, due to their inability to conceive. The entire treatment regimen, which includes travel to India and frequent follow-up appointments, remains financially burdensome. Additionally, the patient reported a significant decline in his physical work capacity compared to his pre- treatment levels.
While surgical excision of the intra-abdominal mass with orchidectomy is mandatory, chemotherapy options depend upon the stage and histological subtype of the cancer11. Our patient underwent excision of the left testicular intra-abdominal mass, right orchidectomy and excision of left para-aortic mass, followed by chemotherapy. Currently, the patient is doing well with no evidence of residual or recurrent cancer based on imaging and tumour marker assessments.
The strength of this report lies in its ability to explore the patient's perspective on the disease, treatment, and its subsequent impact on his quality of life, which distinguishes it from other case reports. However, a notable limitation is the susceptibility to recall bias.
CONCLUSION
Undescended testis is a common congenital anomaly in males which carries a significant risk factor for malignant transformation into testicular cancer. As health care professionals, a thorough physical examination of the genitalia is absolutely crucial when indicated, as the absence of testes in the scrotum can provide an early clue to the diagnosis. Combined with imaging, this plays a crucial role in accurately diagnosing and managing intra- abdominal testicular cancer.
REFERENCES
1.
![]() Wood HM, Elder JS.
Cryptorchidism and testicular cancer: separating fact from fiction. J Urol.
2009;181(2):452-61. [PubMed] [Full Text] [DOI]
Wood HM, Elder JS.
Cryptorchidism and testicular cancer: separating fact from fiction. J Urol.
2009;181(2):452-61. [PubMed] [Full Text] [DOI]
2.
![]() Mohamed YG, Salad NM,
Elmia AM, Ali AM. Intra- abdominal mass with empty scrotum in adult male
revealed as testicular seminoma: A case report. Radiol Case Rep. 2022
11;17(9):3308-3311. [PubMed] [Full Text] [DOI]
Mohamed YG, Salad NM,
Elmia AM, Ali AM. Intra- abdominal mass with empty scrotum in adult male
revealed as testicular seminoma: A case report. Radiol Case Rep. 2022
11;17(9):3308-3311. [PubMed] [Full Text] [DOI]
3. Nkembe MN, Mvalo CM, Tianyi FL, Demba C. Ambiguous presentation of an intra-abdominal testicular seminoma in a 40-year-old man: a case report. J Med Case Rep. 2019 4;13(1):2. [PubMed] [Full Text] [DOI]
4. Paudel S, Kayastha P, Suwal S, Singh SS, Gautam B, Chataut
D. Retroperitoneal Seminoma in Undescended Testis: A Case Report. Nepal J Radiol. 2022;12(2):33-37. [Full Text] [DOI]
5. Ja Jeong M, Hee Kim S, Kim JY, Hyun Kim S, Hae Lee J, Kang MJ. Radiological clues for diagnosing intra-abdominal seminoma in undescended testis on computed tomography. Radiol Case Rep. 2022 26;17(6):2273-2276. [PubMed] [Full Text] [DOI]
6. Leslie SW, Sajjad H, Villanueva CA. Cryptorchidism. In: StatPearls. StatPearls Publishing; 2024. [PubMed] [Full Text]
7. Carlotto JRM, Colleoni-Neto R, Shigueoka DC, Artigiani- Neto R, Lopes-Filho G de J. Intra-abdominal seminoma testis in adult: case report. Arq Bras Cir Dig São. 2015;28:296-
296. [PubMed] [Full Text] [DOI]
8. Miller FH, Whitney WS, Fitzgerald SW, Miller EI. Seminomas complicating undescended intraabdominal testes in patients with prior negative findings from surgical exploration. AJR Am J Roentgenol. 1999;172(2):425-428. [PubMed] [Full Text] [DOI]
9. Lim YJ, Jeong MJ, Bae BN, Kim SH, Kim JY. Seminoma in undescended testis. Abdom Imaging. 2008;33(2):241-243. [PubMed] [Full Text] [DOI]
10. Karcaaltincaba M, Kaya D, Ozkan OS, Akhan O. Preoperative multidetector computed tomography diagnosis of a seminoma originating from an undescended testis by “testicular vascular pedicle” sign. J Comput Assist Tomogr. 2006;30(5):794-795. [PubMed] [Full Text] [DOI]
11. Faruk M, Palinrungi MA, Kholis K, Syahrir S, Bakri S, Azis A. A giant intra-abdominal right testicular seminoma in a bilateral undescended testicle: a case report. Pan Afr Med J. 2023;44:3. [PubMed] [Full Text] [DOI]